What do we know about COVID-19 in kids now?
WHYY’s Health Desk Help Desk looked at the numbers, treatment trends, and patient outcomes.
Listen 4:06
Donald Cucuzzella, 14, of Burlington, N.J,, accompanied by his parents, Holly and Donald, is among the first children to receive the Pfizer COVID-19 vaccine at the Burlington Country mega site in Moorestown. (Emma Lee/WHYY)
Ask us about COVID-19: What questions do you have about the coronavirus and vaccines?
This is one of a series of articles in which reporters from WHYY’s Health Desk Help Desk answer questions about vaccines and COVID-19 submitted by you, our audience.
What do we know today about COVID-19 in kids, many of whom are still not eligible to be vaccinated? Here’s what the numbers tell us.
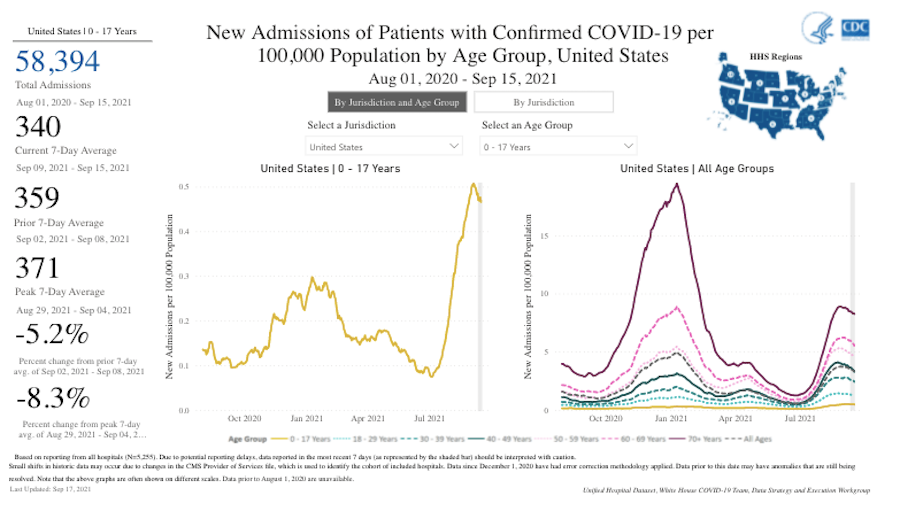
Among children ages 17 and under, cases of COVID-19 and hospitalization have increased, seemingly just as the delta variant became predominant and people returned to their “normal” activities. Between July and the beginning of September, data from the Centers for Disease Control and Prevention shows, there was a sharp spike in pediatric COVID-19 hospitalizations, with a slight dip in the past two weeks. Between Aug. 1 and Sept. 14, there were 58,009 pediatric hospitalizations nationwide.
A CDC study published earlier this month found that hospitalization rates were 10 times higher among unvaccinated kids than among fully vaccinated kids.
The Pfizer vaccine is authorized for use in children 12 and over. Clinical trials have been underway for younger children, and Pfizer said Monday morning that it plans to apply for FDA emergency use authorization for children 5 to 11 by the end of this month.
Since the start of the pandemic in early 2020, there have been more than 4.5 million coronavirus cases among people under age 18 in the United States; 543 kids have died. At more than 2.3 million, the largest number of pediatric COVID-19 cases are among children under 12, who are not yet eligible to be vaccinated. A CDC study finds that pediatric hospitalizations were three times higher in states with lower vaccination rates.
Scientists still don’t know whether the delta variant causes more severe illness in children than other coronavirus variants. But it’s possible that this summer’s rise in pediatric hospitalizations could be because delta is more contagious. One CDC study finds that new pediatric COVID-19 cases increased at the same time delta became predominant in the U.S.
After an earlier spike back in January, COVID cases in the age groups 0-4, 5-11, and 12-17 had declined significantly — to a low in June of 1.7, 1.9, and 2.9 per 100,000 people, respectively. But those numbers spiked again in August, reaching 16.2, 28.5, and 32.7 per 100,000 people, respectively, in those age groups.
During the week ending Aug. 14, the weekly COVID-19–associated hospitalization rate per 100,000 people under 18 was nearly five times the rate during the week ending June 26, according to a CDC study.
“Because [delta] is more transmissible and children are a larger group that are unvaccinated because they haven’t been able to get vaccinated, they continue to be at risk,” said infectious disease specialist Dr. Emily Souder, of St. Christopher’s Hospital for Children in Philadelphia. “And so we worry about getting that group protected and doing all we can to protect them from getting sick and requiring hospitalization, and even just them getting sick and then transmitting it to others who may be immunocompromised or too young to be able to be vaccinated.”
Though children are becoming seriously ill at lower rates than adults are, they still make up a significant proportion of infections and hospitalizations.
But the physicians interviewed for this article say most children who are hospitalized recover and are able to be discharged within several days.
How many kids are affected in this region?
In Delaware, COVID-19 rates per 100,000 in the 5-to-17 age group went from 377 on Jan. 1 to 1,100 on Sept. 15. In total, there have been 20,348 COVID-19 cases among kids under 17 in Delaware.
Physicians at Nemours Children’s Hospital, Delaware in Wilmington have seen an increase in cases among its pediatric population over the past month. Dr. Karen Ravin, division chief of infectious diseases at Nemours, estimated that current hospitalization numbers are closer to what they were in January and February, when cases among kids hit a peak across the U.S. She said Nemours has mostly been treating patients over 12 who are not yet vaccinated.
Similarly, St. Christopher’s is seeing more children test positive both in its outpatient setting and in its emergency room. And overall, there has been an increase in the number of patients being admitted with acute COVID, Souder said.
In Pennsylvania, there were 7,215 new COVID-19 cases among kids ages 5 to 18 between Sept. 8 and 14. As of Sept. 14, there has been a total of 19,838 cases among this age group.
Data from Philadelphia shows trends for people under 20: The infection rate hit a low of 0.9 per 10,000 on June 6. By Sept, 5, it had climbed to 12.2 per 10,000.
New Jersey does not publish trends by age, but the data shows that there have been 126,145 total COVID-19 cases among kids 17 and under and 1,458 hospitalizations since the start of the pandemic.
What accounts for increased pediatric hospitalization rates?
There are many factors, the physicians said, the delta variant among them.
“We know that delta is the primary variant that we’re seeing across the country, and especially including here in Philadelphia. And so that variant is much more transmissible. And I think that’s definitely added to the increasing numbers that we’re seeing,” Souder said.
Vaccination rates for kids between 12 and 17 also have been slower than health experts had hoped for. Just over 41% of children between 12 and 15 have been fully vaccinated, and fewer than 50% of 16 and 17-year-olds in the U.S have gotten a full course of the shots.
Plus, a significant proportion of adults are unvaccinated, which makes kids more susceptible.
“The more adults who get infected, the more risk there is for them to expose kids who are still vulnerable, either because they’re not vaccinated yet, they haven’t had the opportunity to, or they’re not eligible yet,” Ravin said.
Increased social activity may be contributing to the rise in COVID-19 cases and hospitalizations among kids, the physicians said. Unvaccinated people also aren’t wearing masks as frequently as they used to, Ravin has surmised.
“When, earlier in the summer, the recommendations were if you were fully vaccinated, you could go without a mask, I think everybody kind of took that advice and said, ‘Well, if everybody else is taking their mask off then I’m going to too,’ whether or not they were actually vaccinated,” she said. “So we saw a lot of people out and about in the community and returning to their quote unquote, normal lives: Getting out and visiting with other people, being in larger groups of people, going on vacation, traveling, all of the things that people have been longing to do because they’ve been cooped up for so long with the pandemic.
“But, in doing so, there was still COVID circulating in the community, and then with the increase in the delta variant, certainly that had an impact. So people are not following the mitigation strategies that were set forth, which includes masking and keeping your physical distance, and things like that, staying away from crowds.”
What about in-person schooling?
Some schools have had to return to remote learning after coronavirus outbreaks. But Ravin said in-person classes can be conducted safely if precautions are implemented correctly.
“We know what we can do to keep kids safe in a school setting … and that includes things like masking, physical distance, improved ventilation, testing strategies, and the like,” she said. “So we know how to do it safely. I think we still can. And it also really involves vaccination. Everyone who is eligible should get vaccinated — that will help protect our kids who are unvaccinated.”
Souder said vaccination benefits children on many levels.
“Millions of doses have been given in the United States, and there’s ongoing surveillance of long-term outcomes. And from what we know in the last year of information is it’s very safe and it protects you against severe disease and hospitalization and death,” Souder said. “And so I think it’s important as a protective measure for children, and it also helps us get back to a more normal life for children as well. They’re affected when they get exposed to somebody in school, they then have to quarantine, stay at home. So even if they’re not being hospitalized, it is affecting children in other ways, too.”
How has the risk of transmission and infection for kids changed?
It’s still true today that, overall, kids are at a much lower risk for severe disease if they contract COVID-19 than adults are, Souder said. But COVID cases among kids are increasing across the country, which is leading to more hospitalizations.
“We’ve always known that children can get COVID and that they can spread it. We’ve just learned more as time has gone on,” Souder said. “But they absolutely are at risk for getting it, although most do have mild or asymptomatic disease … Over time, we’ve learned more about the virus, and it’s not necessarily that it’s changed among children. I think we’re just more informed and there’s just more cases. So we’re seeing more overall hospitalizations.”
The notion early on in the pandemic that kids rarely get COVID-19 or get severely ill from the virus must be put into perspective, Ravin said. Fewer kids were getting coronavirus early in the pandemic simply because people’s lifestyles were different, she said.
“The things that we have to remember is that when this all started, what did we do? Well, we closed schools, we pulled kids out of school, everybody stayed home. And I have to give credit to all the moms and dads for keeping their kids safe. They kept them home. Nobody went anywhere. You didn’t do anything. You brought your little ‘quaranteam’ group together. You saw just a couple people. You did everything on Zoom. And I think all the things that we all did really helped keep our kids safe and kept them from getting infected early on,” Ravin said.
“What’s different now? Everybody is out and about. So you’re not just in your ‘quaranteam’ anymore with your close contacts. People are seeing multiple different people, people are traveling, they’re getting on planes, they’re driving different places, they’re going on vacation, they’re visiting relatives, going out to eat, going back to church, going back to school. We’re coming into contact with so many more people,” she said.
“So I think that puts us in a different place. And now I think we’re seeing that kids can become infected, obviously, with COVID, they certainly can transmit it. They are at lower risk for serious illness from COVID and from hospitalization and death, but they’re not at no risk. And I think that’s the important part to this … kids are getting this, they are getting sick. Fortunately, they’re not becoming seriously ill and getting hospitalized or dying from this in as high a number as adults, but it certainly is impacting them.”
How are physicians treating pediatric COVID patients?
There haven’t been a lot of treatment studies specifically focused on pediatric patients, Ravin said, so physicians have had to glean information from adult studies and put it into context for kids. Corticosteroids and remdesivir are the two mainstays of treatment. For patients who need additional immune modulating drugs, the two medications being used are tocilizumab and baricitinib.
How are kids doing after COVID?
Some have developed long COVID or post-COVID symptoms, but most kids who are hospitalized recover and are able to be discharged within several days, the physicians said.
“Generally, the pediatric patients have fewer comorbidities and other medical problems. So they are healthier than older adults,” Ravin said. “But they still need long-term follow-up. And that’s one of our goals, is to really, overall for pediatrics, is to try to figure out if there are any long-term potential complications from that infection in pediatrics. And there are hopefully some research studies that look at that.”
Ravin said the one thing she and her colleagues are holding their breath on is whether there will be a spike in cases of MIS-C (multisymptom inflammatory syndrome-children) that correlate with the recent surge of COVID-19 cases.
Previously in the pandemic, the peak for the MIS-C cases came several weeks after the COVID case peak. MIS-C is a rare but serious disease found in children and adolescents that typically becomes evident weeks after the onset of COVID-19. MIS-C can cause serious gastrointestinal, heart, and neurological problems.
Do we know more about myocarditis in young people?
In June, health officials deemed mRNA vaccines (Pfizer and Moderna) safe following more than 300 verified cases of myocarditis, a rare heart inflammation, among 12- to 29-year-olds in the U.S. that were believed to be related to vaccination. At that time, more than 140 million people in the country had been fully vaccinated with the Pfizer and Moderna vaccines. Most of the myocarditis patients recovered from their symptoms quickly.
A study from the University of California that is not yet peer reviewed suggests boys ages 12 to 15 with no underlying medical conditions are four to six times more likely to be diagnosed with vaccine-related myocarditis than hospitalized with COVID-19 over a four-month period. Souder and Ravin said the study should be taken with a grain of salt until it is peer reviewed.
“The American Academy of Pediatrics and the Advisory Committee on Immunization Practices at the CDC have stated that the risks of myocarditis following COVID-19 vaccinations in that age group are very rare, and that if it does happen, it appears to be mostly mild and that patients recover fully. The risk of complications from COVID-19 infection far outweighs any potential risks from the vaccination itself,” Ravin said.
What can parents do?
Parents should encourage everyone in the family to be vaccinated if they’re eligible, and make sure their kids wear masks in public, particularly indoors or in crowds and at school. Kids should also avoid crowded areas, particularly in regions with high rates of community transmission, the physicians said.
“I know everybody’s anxious to get back out and do things that they haven’t been able to do for a long period of time. But I do think there’s ways to do those activities safely. Masking is definitely one, particularly for those who are unvaccinated, and improved ventilation, testing, and it’s always good to wash your hands,” Ravin said.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.





![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)



