Rebooting care: Patients, doctors and dentists catch up after the COVID delays
It will take a while to work through the backlog, because of social distancing and testing issues. But postponed procedures are being rescheduled.
Listen 2:06
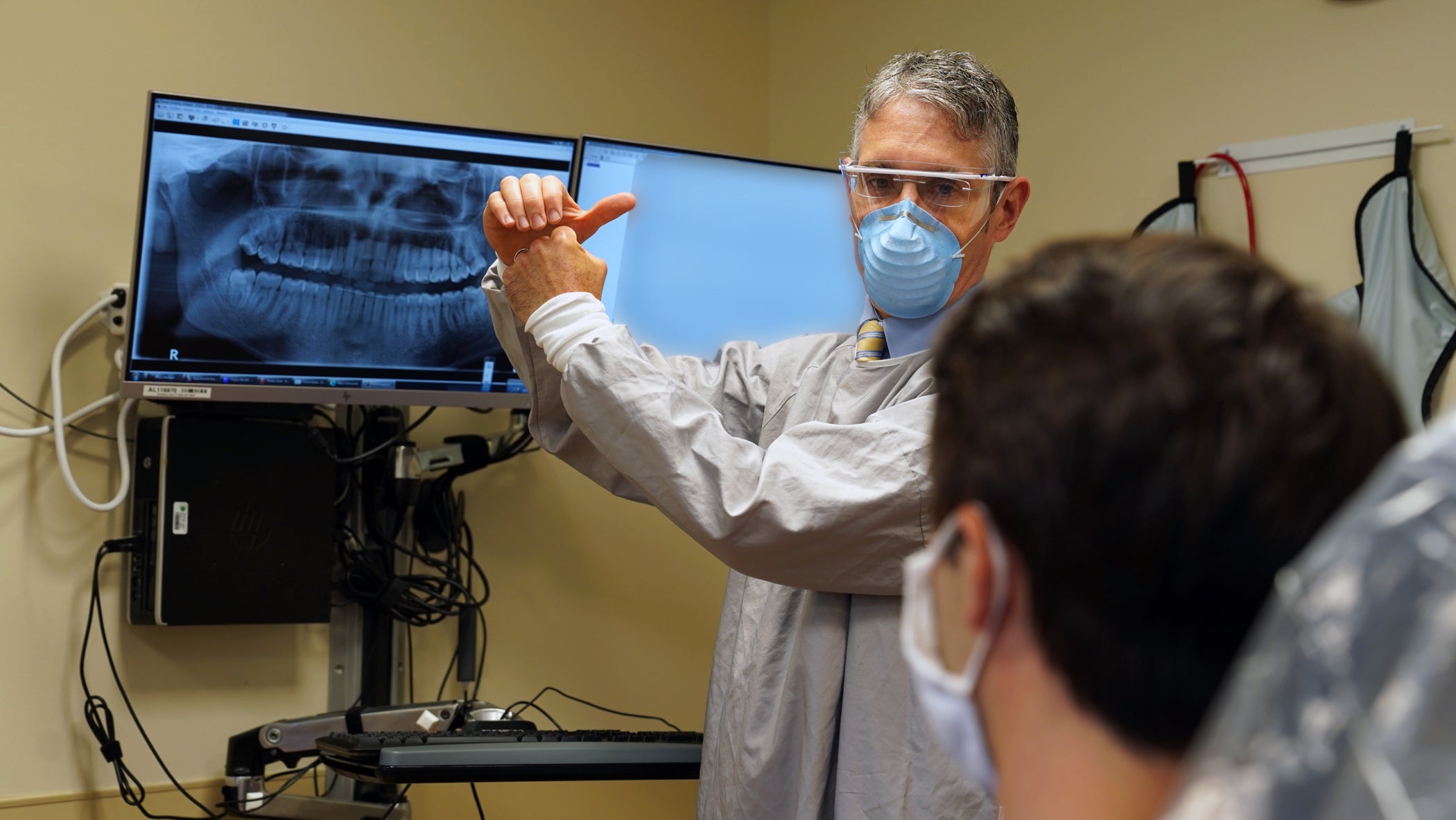
Dr. Dan Meara examines a patient. (Provided by Christiana Care)
Are you on the front lines of the coronavirus? Help us report on the pandemic.
Colin Clifford has macular degeneration in his left eye and needs injections every eight to 12 weeks to prevent swelling and bleeding. The 62-year-old Wynnewood resident lost his right eye in an accident when he was 5.
So as coronavirus restrictions were imposed earlier this year and Clifford’s injection was delayed several weeks, his ability to see was hampered.
“It had been improving month after month after month, but because I didn’t go to the appointment that time, it had deteriorated,” he said. “I couldn’t see very well, my vision was kind of blurry. It didn’t help when I was driving, I couldn’t see distances; the TV was blurry, I couldn’t read my book at night, and I’m an avid reader. So I was having problems.”
“I’m always worried about my eyesight, or having an accident, because if I had an accident my left eye wouldn’t be able to see at all,” Clifford said.
It made sense, then, that after Pennsylvania allowed elective procedures to resume in late April, Clifford scheduled an appointment with his doctor, Dr. Sunir Garg, at Wills Eye Hospital in Philadelphia — even though he felt uneasy about it. Clifford has diabetes, and worries about getting COVID-19.
“My wife has been working from home, my daughter was furloughed at home, my son who is finishing his master’s degree was doing it online, so we’re all at home,” he said. “We’re avid believers in, ‘Stay home and stay alive,’ so we didn’t travel that much. So traveling into central Philadelphia and going into a hospital was worrying. But because of the condition in my eye, it was imperative I did go, so we didn’t have a lot of choice.”
For that first mid-pandemic visit, Clifford said, he and his son arrived at the hospital “petrified,” wearing masks and gloves, and he didn’t know what to expect. Once inside, however, his nerves were put at ease.
“You walk in there, they have someone who sanitizes your hands, takes your temperature, and sends you up in an elevator. They actually have someone who goes in there and pushes the button and sanitizes the button after they pushed it. So, when you get up there and check in, it’s all set to keep everybody socially distanced,” he said.
Last week, when Clifford returned to Wills Eye for another injection, he noticed there were more patients at the hospital than there were previously, mirroring trends at other nearby hospitals that are rescheduling patients whose appointments were postponed during the stay-at-home orders. Still, Clifford said, he felt safe.
Given the signs that the coronavirus isn’t going away any time soon, apprehension is common among patients, medical professionals in the region say. But they note that the lockdowns gave them time to put safety plans and the appropriate personal protective gear in place to protect themselves and their patients.
And now, the appointment calendars are filling up again.
Getting back on schedule
Elective surgeries and procedures resumed in Pennsylvania at the end of April, and in New Jersey and Delaware in May. Rescheduling them is largely being based on the severity of patients’ symptoms.
It will take a while to work through the backlog the delays caused — social distancing requirements mean cutting back on normal capacity at many hospitals and offices. But several health care professionals said patients whose procedures were postponed are eager to get on track again.
“I’m a little surprised at the interest of patients wanting to get back in the mix,” said Dr. Dan Meara, chair of the department of oral and maxillofacial surgery at ChristianaCare.
“There is a small amount of patients who continue to decline to get care for a concern they have, whether it’s just not wanting to be in an environment like an office or hospital setting, or they realize they may be at higher risk because of age or comorbidities they have,” Meara said. “But the majority group is the one that is back out there seeking care and seems to be pleased with the process.”
Many physicians and surgeons say they consider only procedures like plastic surgery to truly be elective — meaning something that can proceed at any time. So during the height of the pandemic, doctors postponed “non-urgent” or “non-essential” surgeries, while continuing urgent and emergency cases.
“If you have a breast biopsy that’s positive for breast cancer, that case will be scheduled within a week or two, because folks don’t want to, nor should they, wait four months to have the breast cancer dealt with. It’s still considered ‘elective,’ but it’s very time-sensitive, and it’s the time-sensitive nature of what we do that dictates when procedures are done,” said Dr. Gerard Fulda, chair of the department of surgery for ChristianaCare.
At the Delaware-based health system, postponing non-essential procedures resulted in 20% the normal volume of surgeries, which typically is about 8,000 a week. The system has slowly increased surgeries, and is now at 85% of its normal volume.
“Some things can be delayed longer than others — so, if there’s some anxiety on the patient about coming to the hospital and it’s something that can be delayed, that’s probably the best course of action,” Fulda said. “If it’s not something that can be delayed, we have that conversation with the patient to let them know of the screening procedures, the cleaning procedures.”
ChristianaCare’s oral surgeons continued procedures throughout the pandemic for problems causing pain or swelling (which can be an indicator of an infection), or involving oral pathology or face trauma. Patients requiring a dental examination pre-surgery also were seen. Now, anyone whose appointments were cancelled or postponed because of coronavirus restrictions is being scheduled at the Oral and Facial Surgery Center, as are people with severe medical issues.
“Gum disease or periodontal disease can lead to chronic inflammation, link to cardiovascular disease, link to preterm labor, link to a variety of comorbidities. Patients who are more medically compromised, have more advanced disease, even if it’s not considered urgent disease — those are the types of patients we are looking at,” Meara said.
Addressing the backlog of cases has been one of his department’s biggest challenges, Meara said. “Every day, there’s walk-ups coming in that are deemed urgent, and new patients that want to seek care here. So it’s a balance of having opportunities for all those groups to seek care at the same time.”
Orthodontists handle more aesthetic procedures, like braces. Dr. Ray Rafetto, of Alpine and Rafetto Orthodontics located across Delaware, said his office has resumed procedures at about 65% of its normal volume. Because of social distancing requirements, he doesn’t think volume will increase any time soon.
About 60% of his patients who had already begun procedures were itching to get back to them, Rafetto said, because most straightening treatments take roughly 12 to 18 months to complete. Another 30% felt safe rescheduling their appointments only after learning about the safety protocols.
And the other 10% said, ‘“You know, I’m not going to die of crooked teeth, I’m OK waiting until times are a little safer,’” Rafetto said.
Prioritizing care
Dr. Dorothy Moore, an ophthalmologist with Delaware Eye MD Associates in Wilmington and the past president of the Medical Society of Delaware, said scheduling procedures often depends on how poor a patient’s vision is.
“Some patients have had their cataracts put off for several months, and their vision is worse than it was previously. For my strabismus patients, and these patients have double vision, and we’ve now put off their surgery for their double vision for several months, they’re certainly anxious to get that done,” said Moore, who also practices at Nemours Alfred I. duPont Hospital for Children and at ChristianaCare.
Delaware resumed non-urgent eye surgeries only three weeks ago, Moore said, and she has recently started setting up procedures for between the end of July and September.
Moore specializes in pediatrics, and not many of her patients have been reluctant to reschedule, she said.
“You don’t want to put kids off too long because then you run the risk of having issues with their binocular function. The parents were pretty accepting in getting their surgeries,” she said.
Wills Eye Hospital is inching closer to its normal capacity every day. Dr. Michael Cohen, a retinal specialist, said he has seen some negative consequences when patients delay their own care.

“There was a patient I had today who started having visual symptoms. He had a bunch of underlying eye diseases already, but he had symptoms starting at the end of March or April. He was a few states away and was reluctant to get care, and ended up having a retinal detachment, which is a relatively urgent thing that needs repair,” Cohen said. “He has a much more guarded prognosis now, four months sitting with a retinal detachment, than he would have had if he sought care earlier.”
Penn Medicine ramped up surgeries at the beginning of May, implementing a prioritization process with a scoring system developed by the University of Chicago. The scoring system evaluates patient factors such as age, comorbidities, potential alternatives to surgery or if there’s a possibility of adverse outcomes if surgery is postponed.
Surgeons at Penn Medicine say their biggest concern is the potential for adverse outcomes, especially for patients with a malignancy.
“We were very careful, even throughout the pandemic, to follow the American Cancer Society guidelines and make sure if a patient had advanced cancer, we actually performed the surgery,” said Dr. Deborah Driscoll, senior vice president of clinical practices at the University of Pennsylvania. “But if it was an early stage and not likely to progress, we felt comfortable deferring it for a couple months. I’m not aware of any patients that had an adverse outcome because we delayed surgery.”
Several thousand surgeries at Penn Medicine were deferred. Each surgeon in the health system is responsible for reviewing their cases and prioritizing them.
“Many patients have rescheduled their surgery, and they really appreciated that their physicians called them and that we were available to take care of them,” Driscoll said. “There are some patients who felt they wanted to wait a few months; they didn’t feel an urgent need to have their procedure.”
Dr. Peter Abt, a professor of transplant surgery for Penn Medicine, said he’s aware of about three or four times that patients waiting for kidney transplants refused the organs during the spring, because they didn’t want to risk going to the hospital. That is no longer happening, he said.
Postponing a kidney transplant doesn’t change a patient’s place on the waitlist, and these patients are usually on dialysis, which can afford them more time to postpone, Abt said. “So, it may be that they think, ‘Well, I’ll wait a few more weeks and the COVID pandemic will calm down a bit and then I’ll come in for my transplant.”
But he added that there are several reasons why a patient might refuse a kidney transplant, in addition to the fear of contracting COVID-19 at the hospital or from the organ they’re receiving — something Abt said he is not aware has ever occurred. For living-donor transplants, Penn Medicine requires donors to quarantine for two weeks prior to donation, and they also are tested twice for the virus.
“Once they have that transplant and leave the hospital they’re immunosuppressed, so, ‘What’s the risk of contracting COVID in the community?’ And then there’s another piece … we’ve been limiting visitors to the hospital during the pandemic, and many patients want to have their loved ones with them during their transplant,” Abt said.
Layers of precaution
In addition to social-distancing measures, hospitals are asking patients to wait in their cars until they’re called in, screening patients for COVID-19 symptoms before they enter the building, and enforcing mask-wearing.
“I think the more people hear about the steps being taken, the more comfortable people feel. But everyone has their own level of risk they’re willing to take, and I think it’s just a matter of getting people to a place they feel comfortable seeing their doctor,” said Dr. Cohen of Wills Eye. “Patients have to be able to feel comfortable with the decision. No one should make a decision that they don’t feel is in their own best interest, or potentially look back and say, ‘I wish I did things differently.’”
The only setbacks Wills Eye has faced, Cohen said, revolve around issues with testing, which is required before surgery.
“In the early stages, it was a little tough to get those tests; it’s getting better now. It’s still not perfect, depending on where patients go. That may be the biggest hiccup,” he said. “We’re plugged in with Jefferson, and they’ve been pretty great with their turnaround time. There are some places where I have to get tested before I operate, and they had my results in 12 hours. But there are still some patients of ours that have gone [to other places], and it’s taken them six days to get their results back.”
For dental procedures, which require patients to remove their masks, oral surgeons have additional safety precautions to consider.
“If they are scheduled for a procedure that’s at high risk for creating aerosols, which … mix droplets into a mist and can travel a great distance, if the procedure is likely to generate an aerosol, then they have to be COVID-tested before they come in,” said Dr. Meara of ChristianaCare.
“Even if it’s not a procedure that’s going to generate aerosol, if they’re having anesthesia they have to get COVID-tested within 72 hours, because there’s potential for airway manipulation,” Meara said.
Dr. Rafetto said his office has set aside certain areas for aerosol appointments, which in orthodontics are typically limited to putting braces on and removing them.
One of the biggest issues Rafetto’s office faced when elective procedures resumed was not having enough gowns, which are required for aerosol procedures. He said his office has gowns today, but for a while had to postpone several procedures because there weren’t enough.
In Pennsylvania, some dentists’ offices are charging patients a PPE fee because shortages have increased costs. The American Dental Association and the Pennsylvania Dental Association have been advocating for insurance companies to cover some or all of those costs, according to a spokesman for the state group.
Both Rafetto and Dr. Moore, the Delaware ophthalmologist, said patients should expect safety protocols to become the new normal — which could mean a change in scheduling because they’re seeing fewer patients to keep everyone safe.
Raffetto added that lessons learned so far during the pandemic have been valuable.
“I think the cross-contamination protocols are a good thing, and it’s been an amazing learning experience,” he said. “Just a simple thing, when we were coaching our staff weekly through the pandemic when we were closed, I realized how much I touched my face. And washing our hands for 30 seconds — 30 seconds is a lot longer than what I was typically doing.
“So, a lot of good things have come of it in the big picture, and an awareness everyone has of how viruses can transfer,” Rafetto said. “I’m still astounded how little virus particles could paralyze the world in the fashion they have.”
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.




![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)

