‘Combat fatigue’ for Del. caregivers as COVID-19 hospitalizations at all-time high
Nurses, hospital directors and public health officials worry that the growing number of patients could overwhelm the system and caregivers.
Listen 2:07
Dr. David Tam of Beebe Healthcare (center with black mask) says his staff is suffering from "combat fatigue'' while battling the pandemic and treating patients with other medical needs. (Courtesy of Beebe)
More COVID-19 patients are now hospitalized in Delaware than at any time during the nine months of the pandemic.
For now, with patients not getting as sick as in the spring and advances in care negating the need for hospital treatment or resulting in shorter stays, health officials say the state still has beds to spare.
But they are rapidly filling up with the daily case average growing almost exponentially. That means increased pressure on the facilities themselves as well as doctors, nurses and other caregivers, which hospital executive Dr. David Tam likens to “combat fatigue.”
Tam, who heads Beebe Healthcare in Sussex County, told WHYY News that Beebe Hospital in Lewes is seeing a steady but not yet alarming increase in coronavirus patients but worries the number could eventually overwhelm Beebe or force them to delay other non-essential treatment for patients with other physical ailments.
Tam also said stress on the statewide system and others in the region could also prevent Beebe from sending patients needing a higher level of care to Christiana Care’s two larger hospitals in northern New Castle county, or to ones in Baltimore or Philadelphia.
The former Navy man used the military analogy to urge Delawareans to take precautions to stop the spread of the virus.
“It’s like combat fatigue,” Tam said. “We call it pandemic fatigue for our staff. It’s a war on COVID and they’ve been on the front lines now for nine months straight. We need help from the home front. It’s like back in World War II. Remember how people back home were doing anything possible to help?”
Christiana Care officials would not speak with WHYY about its capacities or COVID-19 patient load.
But chief operating officer Sharon Kurfuerst said in a written statement that “while this virus remains dangerous, our care teams within our hospitals now have proven therapies to help patients recover, and our ambulatory and virtual care teams are providing care to COVID-positive patients who are quarantining at home—often preventing the need for acute care.”
Kurfuerst’s statement said the hospital has “had contingency plans in place for any scenario” since the pandemic began, but did not reveal those plans.
“We believe that we have the capacity to meet the needs of the community throughout the winter. We continue to monitor the data and update the plans that we developed in the spring, in collaboration with the state and the other health systems.”
Nurse on front lines: ‘Everybody is tired’
One nurse who works downstate but requested anonymity because line workers are not permitted to speak to the media told WHYY News that some less-experienced nurses have left their jobs because the pandemic has overwhelmed them, and others have taken jobs as traveling nurses in other areas for as much as $8,000 a week.
Those who remained in their posts are dedicated to patients but heading toward burnout, she said.
“Everybody is tired, not just the staff but families,’’ the woman said. “Families are tired of hearing you can’t do this because of COVID, you can’t allow visitors because of COVID, or ‘Here, I’m going to put you on the iPad so you can talk to the doctor.’
“It used to be the doctor would come around and do rounds and the families would find out, ‘Okay, this is what’s going on with mom-mom. Now you are not able to have as much interaction.”
The nurse is also weary of people who don’t take the virus and prevention measures seriously.
“I can’t stand to hear them say, ‘Oh, it’s just a flu,’” she said. “It’s definitely not just the flu. Is everybody going to get super sick? No, but at the same time people will. The struggles they go through with COVID are different than with the flu.”
While Christiana Care won’t discuss its COVID-19 patient count or how it’s affecting the allocation of beds, one woman told WHYY her cousin’s ambulance trip to Christiana Hospital’s emergency room last week for treatment of his diabetes was rerouted to St. Francis hospital and he was admitted there because Christiana didn’t have room.
And Sherrie Scully told WHYY that she was kept overnight in November recently at Christiana Hospital for a tear of the lining in her vertebral artery, which can cause a stroke.
When Scully, the mother of a young child, was released the next day and told to strictly limit her movements, she said someone on her treatment team informed her she was being discharged because “there were 65 people waiting to be admitted. If it wasn’t for COVID, you wouldn’t be going home today.”

The experience rattled the 41-year-old Scully, who had delayed getting treatment for days while the pain in her neck kept increasing.
“It’s scary,’’ she said. “I didn’t even want to go to the hospital because I’m afraid of getting COVID.”
Christopher Otto, who heads the 25,000-member Delaware Nurses Association, says those who work in hospitals and other places with outbreaks, such as nursing homes and prisons, are reeling under the strain.
“Nurses are expressing concerns around stretched assignments, so taking on more workload and the ability to provide safe quality effective care,” Otto said.
“The second wave is really pushing the limits on nurses in terms of their mental, physical and emotional well-being. Having to go back to quarantining from loved ones. Taking measures to protect themselves, protect their colleagues, their patients. It’s exhausting.”
Inpatient numbers are grim and growing
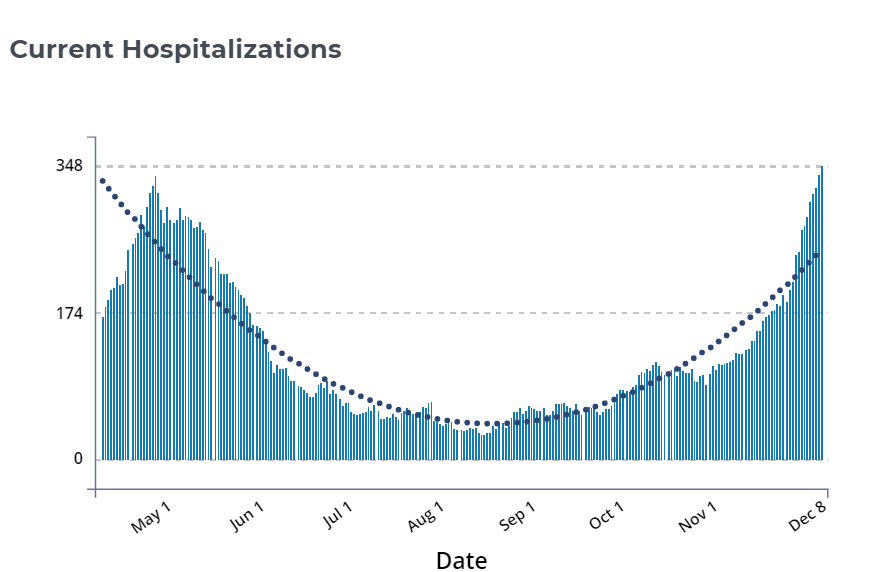
On April 27, seven weeks after Delaware’s first reported coronavirus case, 337 patients were hospitalized. But after a stay-at-home order and other restrictions for much of the spring and part of the summer, by late August that number had fallen to 29.
But with the advent of autumn and restrictions eased, the number of people getting infected began skyrocketing, and the number needing inpatient care started rising.
As of Thursday, the state’s hospitals were treating 349 COVID-19 patients and 44 were in critical condition. That tally comes as the state’s weekly average of new cases daily has hit 810 — four times the figure of just a month ago.
More than 800 Delawareans have died of coronavirus-related causes, health officials say.
Gov. John Carney and top administration officials expect more patients to need hospital care unless residents take strict steps to stop the rampant community spread.
Starting Monday, Carney is implementing a stay-at-home advisory and requiring anybody who spends time indoors with anyone not in their household to wear a mask. Children age 2 and under are exempted from the mask mandate.
A.J. Schall, who heads the Delaware Emergency Management Agency and this week recovered from what he called a mild case of coronavirus, told WHYY News that hospitals have space and staffing to accommodate perhaps another 200 patients, though he said it could be more depending on how hospitals use their space.
But should the patient count get too high, Schall said officials could take measures such as banning elective and non-essential surgeries or setting up an alternate care site with the National Guard.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.




![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)


