Building a pipeline to replenish the supply of primary care doctors in N.J.
A shortage of primary care physicians is projected in New Jersey. A new program offers scholarships to low-income students to pursue those careers.
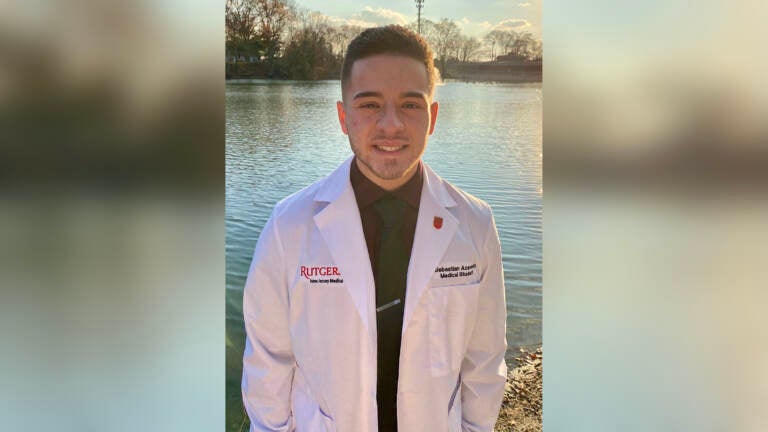
Sebastian Acevedo is a second-year medical student at Rutgers New Jersey Medical School pursuing a career in primary care. (Photo courtesy of Sebastian Acevedo)
Sebastian Acevedo didn’t always know he wanted to be a doctor. He’s currently a medical student at Rutgers New Jersey Medical School, but experiences as a child helping his parents navigate U.S. health care opened his eyes to the system’s many flaws.
When Acevedo was 4 years old, he immigrated with his family to the United States from Colombia. They settled in Ventnor City, New Jersey, where from a very young age, Acevedo said, he served as an informal interpreter for his parents. And when his mother was diagnosed with chronic venous insufficiency — a condition that occurs when your leg veins don’t allow blood to flow back up to your heart — he took on the role of translator between her and the doctors she saw for her care.
“My mother had regular issues that required very specialized care,” Acevedo said. “And being exposed to health care on that scale, you really do get a sense of the complexity and, more importantly, the sense of helplessness that a lot of patients experience, especially when there’s a language barrier.”
His mother, who was undocumented at the time, continued to get more ill, and soon her doctors recommended that she have her leg amputated due to some medical complications. His parents were in immense amounts of debt because of the health care his mother received in this country. So in 2011, Acevedo’s family returned to Colombia, where in the end doctors were able to save his mother’s leg — the leg she had been told here was beyond saving after three years of medical treatment.
Acevedo said he doesn’t believe Colombia has a better medical system than the United States, but when he thinks back on this critical moment for his family, he believes Colombia was able to offer his mother the culturally competent care she was missing in the U.S.
“They were able to understand her complications and, more importantly, how to offer her treatment that met her needs,” said Acevedo. “And this experience sort of helped me understand that health care, especially good patient outcomes, comes by way of not only offering the best medicine available, but doing so in a way that is appropriate for our patients’ socioeconomic and cultural beliefs.”
For many individuals and families in the U.S., primary care is typically the entry to more specialized medical care. The role of a primary care doctor is to advocate for those in need and to be the main medical point of contact
“We become the gatekeepers of the health care system, and we also become the doctor that brings together the thoughts of all of the other doctors in terms of specialty care on behalf of a patient,” said Dr. Ana Natale-Pereira, who has served as a primary care doctor for over 25 years. “We deal with complex care and more importantly, we’re present in a person’s life for the long run.”

But New Jersey is one of a dozen states expected to have the biggest shortage of primary care doctors in the country. The Health Resources and Services Administration projects that 37 states will have a shortage of primary care physicians by 2025, with 12 of them, including New Jersey, having a deficit of 1,000 or more physicians because of the aging American population and the number of doctors nearing retirement.
And a growing number of patients, particularly those who are uninsured, as well as immigrants who lack citizenship, don’t have access to a primary care provider at all. These patients are typically turning to emergency departments for speciality care, which means delayed treatment and higher risk of patient morbidity and mortality.
Natale-Pereira is the assistant dean of primary care and community initiatives at Rutgers New Jersey Medical School.
““Primary care is not just runny noses, earaches and sore throats. We are dealing with incredibly complex care, particularly in underserved communities,” said Natale-Pereira. “Unfortunately, the shortage of primary care physicians in urban areas forces many residents to seek health care from the emergency department or community health fairs, leaving them with no continuity of care.”
In 2017, administrators at Rutgers New Jersey Medical School put together a task force to study the impact the school had on the community at large in New Jersey. What became clear is that there was a scarcity of Rutgers-trained doctors in the primary care network in Newark. In response, NJMS created the Office of Primary Care and Community Care Initiatives in 2020, which brought together research, education, and community service opportunities for students pursuing careers in primary care.
That same year, NJMS launched the Reducing Barriers to Success Scholarship Program, which provides 20 medical students from underserved communities with financial scholarships each year to become primary care physicians in Newark and surrounding towns.
The scholarship program, which covers close to three-quarters of medical school tuition, is funded by a five-year, $3.25 million grant from the Health Resources and Services Administration. The goal is to connect participants with mentors in primary care fields, expose them to research and community engagement opportunities, and allow them to grow a community of other medical students with overlapping career goals.
“They’re usually students that come from communities of color, and what drives them into this space is really that they want to give back,” said Natale-Pereira. “They want to help fix what many of them grew up knowing, [which is] that a [primary care doctor] shortage is there and that there are … inequalities in health care.”
Medical school debt may sway students from primary care
There’s a growing recognition that medical schools nationwide have to grow a diverse medical workforce, Natale-Pereira said. But pursuing a career in medicine can come with a whole slew of barriers, particularly for low-income students of color.
Acevedo, who is in his second year of medical school at Rutgers, said he remembers applying to medical schools before the scholarship program was available. He applied as a full-time student, which meant taking out full-time loans. According to Natale-Pereira, medical students are typically incurring large debt in medical education, which contributes to the observed shortages in primary care medicine.
“Even for the [students who] are interested in going into a primary care field, they look at the [salary gap], and then they say, ‘Well, maybe it’s best for me to go into a specialty program because obviously, you know, finances are much better,’” said Natale-Pereira. “And so the financial side is one of the reasons why there is a shortage there.”
But in 2020, Acevedo, who’s interested in pursuing a career in internal medicine and psychiatry, had the opportunity to apply for the scholarship program. When he got it, he said, a whole family of students who were interested in careers in primary care and bridging health disparities awaited him.
“We have monthly meetings in which we [hear] from physicians that are practicing medicine right now,” said Acevedo. “So the program is really intended to not only drive that interest in primary care, but also allow us to network and think critically about how primary care work looks, especially with communities that have been historically underrepresented in medicine.”
During the pandemic, Acevedo has worked in the medical school’s satellite clinics, which serve, among other locations, two shelters in Newark that help people at risk for homelessness. He serves as a mentor for high school students interested in careers in medicine, and now he’s part of a research group called the Community Health Justice Lab, where he conducts surveys on Latino health and COVID-19 outcomes.
“I’ve been to Camden, I’ve been to South Jersey, and [this project] has driven me to talk to people, specifically Latinos, and get their sense of how COVID is impacting [them] emotionally, financially, socially,” said Acevedo.
‘Being the doctor I wish my family had’
The benefits of a scholarship program like the one at Rutgers New Jersey Medical School are numerous: financial freedom; exposure to new career prospects; professional development. Those are some of the most critical elements for boosting medical students into the careers of their dreams. And for many students who are low income or are the first in their families to pursue higher education, there’s a unique desire to give back to the communities they call home.
Angelica Lopez always knew she’d become a doctor. A South Bronx native, she grew up visiting her family in the Dominican Republic, where she said her uncle, who was a physician there, inspired her to pursue medicine. Like Acevedo, she was constantly translating between Spanish and English for her parents during routine checkups and trips to the doctor’s office in New York City. Shortly after graduating from college, her father passed away during cardiac catheterization, a procedure that typically doesn’t have major risks or complications.
“After he passed, we had a lot of questions, and a big one was actually did [my father] really understand what was going on in that procedure, because he didn’t speak English well,” said Lopez. “And just having those experiences growing up, for me, served as a huge inspiration for wanting to be able to go into medicine and to be the physician who could bridge those gaps.”

Now Lopez, a scholarship recipient, is a fourth-year medical student at Rutgers New Jersey Medical School, where she’s studying to pursue a residency in family medicine. She has staffed a call center, calling patients in the Newark area who had participated in a COVID-19 screening program, educating them on the virus and learning their concerns. Many had language barriers and were isolated or uninsured.
“This allowed me to learn about many of the myths that were going around about the virus,” she said. “As a student, I had the time to talk to patients, often in Spanish, to dispel those myths and to give them resources if they did not have food or shelter or needed a COVID-19 test. These were likely the people who otherwise might have slipped through the cracks.”
Initially, the loans Lopez would have needed to complete medical school caused her a lot of concern. Now, much of that burden has been lifted, and she said she can see her future more clearly.
According to Lopez, primary care is really at the heart of patient outcomes. It’s typically the place where most patients make that first contact with a health care provider. She and Acevedo said they see a lot of potential in primary care to improve long-standing racial and ethnic health disparities.
“The main point in going into primary care for me is being able to be the doctor that I wish my family had when I was growing up,” she said.
—
Support for WHYY’s coverage on health equity issues comes from the Commonwealth Fund.

Get daily updates from WHYY News!
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.








