Temple physicians learn mindfulness to cope with the trauma of treating COVID
Witnessing so much suffering and loneliness took a toll, so Temple Hospital’s Practitioner Wellness Committee sought a program to help.
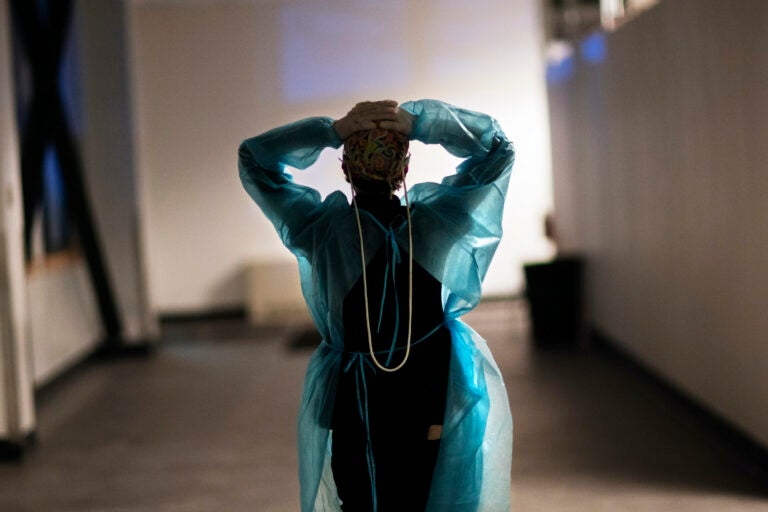
A nurse walks down a hallway during a night shift at a field hospital. (AP Photo/David Goldman)
Through the first month of the coronavirus pandemic, Temple University Hospital obstetrician Stacey Jeronis isolated from her family as much as possible when she came home. The world was still learning how COVID-19 spread, and Dr. Jeronis was terrified her family might catch it from her.
“I’d go home, I would shower and leave my clothes outside, and I really didn’t interact with my family for weeks until I realized that wasn’t sustainable,” she said. “Because the pandemic wasn’t going anywhere.”
Jeronis delivered babies throughout the pandemic. When her pregnant patients came in, they were masked and tested for the virus. But if a test came back positive, Jeronis and her staff still had to deliver the child.
“You’d have a woman coming in with a COVID infection and she could be really sick, and you have to see her, but you also have to limit your interaction with her,” Jeronis said. “And they were alone. They weren’t allowed to bring anyone initially. And that was a lot different than we’d had it in the past, where the whole family would come in to celebrate, and here, everyone was just kind of alone at that time.”

The experience — being routinely exposed to COVID-19 at work while simultaneously fearing she’d infect her family at home — took a severe toll on her mental health, Jeronis said.
“We just didn’t know,” she said. “It was … tough and definitely traumatizing at the time.”
Those on the frontlines of COVID-19 routinely faced immense amounts of trauma treating patients during a global health crisis. But with mental health resources scarce because of the pandemic lockdowns and providers’ increased workloads, many health care workers struggled to find what they needed to cope with the stress of treating patients infected with the virus.
In February 2020, Jeronis became head of Temple’s Practitioner Wellness Committee, whose purpose is to “enhance the culture of wellness” for Temple’s physicians. In her new post, Jeronis saw that many of her colleagues were experiencing the same feelings of isolation and fear. With the pandemic, the committee’s focus shifted from adjusting the health system’s systemic workflow issues to giving physicians tools to be more resilient in light of the “new normal”: always wearing personal protective equipment; keeping themselves safe from infection; and watching many of their patients suffer without loved ones permitted in the hospital to comfort them.
When a coworker mentioned to her that Providence Treatment Center in Media was creating a new program designed to help physicians cope with trauma, Jeronis welcomed the opportunity to bring it to Temple. She got in touch with Dr. Bill Heran, CEO of Providence Treatment, who put together a program predicated on practicing mindfulness to relieve trauma and stress.
During 20 years of experience treating physicians with substance use problems, Heran said, he has found mindfulness — the practice focusing one’s awareness on the present moment — to be an effective technique.
A key tenet of mindfulness meditation is calmly accepting one’s feelings and thoughts without subscribing to them, often through breathing exercises and meditation. Heran had previously taught the practice to Temple medical students.
This time, he created an eight-week course in one-hour sessions, administered over Zoom, that were attended by about 50 physicians looking for ways to manage their work-induced trauma. Each week, from March to May this spring, the doctors attended meetings focused on different types of meditation to provide the tools necessary to cultivate the practice. Temple paid for their physicians to attend the sessions.
“The average physician doesn’t deal with so much death on a daily basis and such an intensity of care,” Heran said. “They had to have difficult conversations with family members who were unable to visit their loved ones in the hospital. This was a fairly new behavior for physicians, and it caused a greater degree of stress.”
Another important part of mindfulness is focused breathing exercises.
“If a doctor is seeing a patient, and maybe takes 30 seconds to breathe before they get into the exam room, that makes them more present. So when they open the door to treat a patient, there’s much more of a clearing,” Heran said. “It allows them to focus on the here and now without all that story and without judgment.”

Dr. Christina Chu, a gynecologic oncologist, said practicing mindfulness allowed her to be less judgmental of herself while treating patients infected with COVID.
“My job has always been stressful, and my personal life has always been stressful. But the stress this year has been different,” she said. “I spend a lot more time on the phone with family members of patients because they can’t be there in person.”
Chu was also nervous about bringing COVID to her family, specifically to her mother, an 80-year-old two-time cancer survivor. During the sessions with Heran, Chu used different objects to meditate on and listened to outside speakers who talked about employing mindfulness to stave off stressors and negative thoughts.
Since the course was offered after the peak of the pandemic, sessions often focused on how to deal with the residual mental effects of treating COVID patients. Those in the sessions were struggling to recover from their trauma and needed tools to compartmentalize to continue to do their jobs and maintain stability in their family lives.
“At the height of the COVID crisis, we were limiting visitors. It was hard when patients were dying, and we sometimes could spare a nurse so they wouldn’t be alone, but it was just heartbreaking for patients and families,” Chu said. “It’s heartbreaking for the nurses, for the staff. It’s been really difficult.”
Chu said the more she practices meditation, the better she gets at compartmentalizing the trauma of watching her patients suffer alone.
“It’s a process. When COVID would prevent me from doing my job properly, I have these thoughts that I’m an awful doctor. I feel worse than dirt,” she said. “How I dealt with that before was that I’d think about it, push it down, suffering internally, and eventually it just gets pushed down and contained somewhere.”
Now, she’s learning how to prevent her stressors from bringing down her own self-worth, which negatively affects both her personal and professional lives.
“Now, I’m trying to recognize, ‘Yes, this is stressful and sad,’ but it’s not a switch I can turn on and off. I’m practicing separating that baggage from these negative thoughts,” Chu said. “You become a doctor because you have compassion and you want to help people … Even when you do everything right, sometimes, you can’t prevent a negative outcome.”

With COVID restrictions eased in Philadelphia, visitors are allowed at hospitals again, and fewer patients suffer and die from COVID complications. Still, Chu said, she continues to practice mindfulness to manage the feelings of sadness and isolation she experiences coming out of the pandemic, and rebuilding her self-worth as a doctor.
But these days, she’s learning not to succumb to her trauma, one deep breath at a time.
Jeronis, who participated in the sessions, said that through the breathing exercises and guided meditations, as well as talking with other physicians going through the same thing, she was better able to reconcile her trauma.
“Some of the things [Dr. Heran] said that really made a difference were to be in the present, not think about past or future,” Jeronis said. “A lot of our worries aren’t as bad as we think they are, and I needed to learn to be nonjudgmental of my thoughts and feelings, and just be.”
Now, she said, she chooses to focus on “acceptance and gratitude” to better cope with the horrors of the pandemic.

Get daily updates from WHYY News!
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.





![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)


