Rethinking advice amid COVID summer surge: How long do you really need to isolate?
If you Google COVID isolation standards, you're likely to get a few different answers. So which one should you follow?
Listen 1:09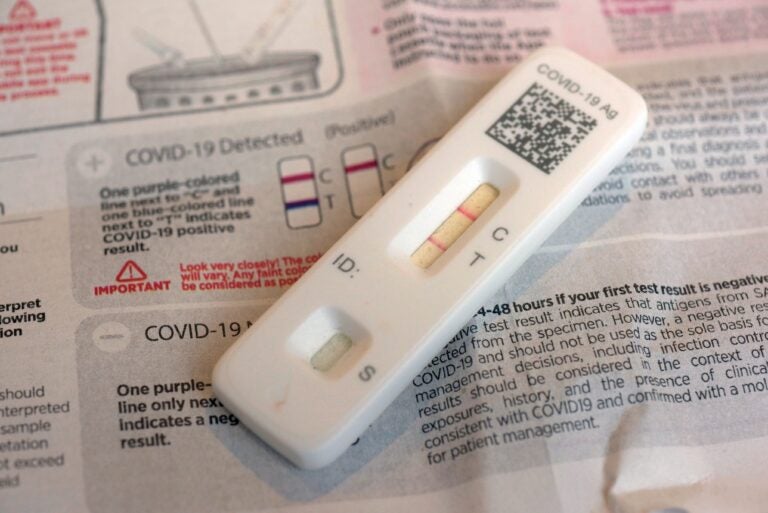
A COVID-19 antigen home test indicating a positive result are photographed in New York on Wednesday, April 5, 2023. (AP Photo/Patrick Sison)
From Philly and the Pa. suburbs to South Jersey and Delaware, what would you like WHYY News to cover? Let us know!
It’s been a while since most of us have had to think about masking or isolation. But according to wastewater data from the Centers for Disease Control and Prevention (CDC), the U.S. is currently experiencing a major surge in COVID-19 cases, with more than half of states reporting “very high” levels of viral activity, and Pennsylvania reporting “high.”
“What is clear is that we are in the middle of a very large summer surge — and that was not anticipated,” said Neil Fishman, an infectious disease physician and chief medical officer at the Hospital at the University of Pennsylvania. “What I anticipate happening, based on what we’re seeing in the West Coast, is that there’ll be some steady but high-level activity that’ll begin to tail off over the next several weeks.”
Until then, what can we expect from the newer variants, and what’s the best way to keep ourselves — and those around us — safe?
FLiRT Variants
The most dominant strains right now are known as the FLiRT variants — and although we may have less resistance to these variants, due to their mutations, Fishman says they aren’t any more severe or contagious than previous iterations of COVID-19.
“They appear to cause the same type of disease as other strains,” Fishman said. “So mild to moderate respiratory viral infections in most people.”
However, he added that symptoms can be much worse for those who are unvaccinated, very young, elderly, immunocompromised, or have underlying diseases, especially lung diseases, as it was with past COVID-19 variants.
But that doesn’t mean people who don’t fall into those categories have nothing to worry about.
“The one thing we do need to remember about COVID or other diseases as well — influenza, for instance — is it’s still a serious infection,” Fishman said. “And it will likely kill or be responsible for the death of about 50,000 people this year. And that’s significant.”
People should also keep in mind that older vaccines become less effective with the newer mutated variants.
“They do provide some protection, but not as much protection as they did to the strains they were directed towards,” Fishman said. “The new vaccine that’ll be available in the fall will be much more effective against the newer variants.”
Existing at-home tests are equally effective as before at detecting the newer strains, but may not provide a positive result until a few days after contracting the illness, Fishman said.
“In some of the newer strains, it appears that the home tests may not become positive until a little later in the course of the illness — day three, for instance,” Fishman said. “So, if someone tests negative and believes they still have COVID, I would do another test the following day and maybe even a third day to see if they do have COVID.”
How long do you really need to isolate?
Over the past few years, the CDC has changed its COVID isolation guidelines twice — first decreasing the standard from 10 days to five days in 2021, and earlier this year, replacing the five-day guideline with advice to isolate until you’ve been fever-free for at least 24 hours and when your symptoms have improved.
It’s a guideline that’s being followed by some of the biggest employers in the Philadelphia area, including Temple University, Aramark and the Philadelphia school district.
But some experts have criticized the new standard as overly lax, and the CDC admitted that both changes were influenced by practical concerns, like interruptions to essential services, and what guidelines the public would actually be willing to follow.
So how long are we actually contagious with COVID?
“It varies,” Fishman said. “A lot of different factors contribute to how long a person is contagious, and they include an individual’s immune response to the infection, whether or not they were vaccinated and whether or not they take a drug like Paxlovid to treat the infection.”
In general, Fishman said that the risk of transmission does decrease significantly when a fever is no longer present, a fact that supports the CDC’s latest recommendation. But, he added that the risk doesn’t drop to zero.
“The risk decreases significantly after day five, if there are no symptoms,” he said. “But really, there is some minor risk of transmission likely through day 10.”
Five days seems to be the magic number, Fishman said. A 2022 study conducted by researchers at Imperial College London found that among the 42 cases they tracked, peak infectious viral load occurred at a median of three days after symptom onset, and the median duration of infectiousness was five days. In other words, 65% of cases remained infectious at day five, and 24% were still infectious at day seven.
However, Fishman said that it’s important to keep in mind that levels of infectiousness decline over time.
“The concentration of the virus is significantly important in transmission,” he said. “So the concentration of the virus that’s shed is, in day five and certainly day seven, much lower than early in the infection. So the risk of transmission is significantly lower.”
That’s why they allow health care workers to return to work on day six if they no longer have symptoms, he said, though they’re required to mask through day 10.
Best practices for those living or working with vulnerable populations
Similar advice applies to anyone who lives or works with vulnerable populations, like the elderly or immunocompromised.
The first and most important recommendation, Fishman said, is to stay home when you’re sick to avoid infecting others.
If you’re not sure whether or not you’re well enough to break isolation, do several rounds of testing.
“You should test at least twice, two days in a row, 48 hours — maybe three days in a row,” Fishman said. “And during that at-risk period, if you’re not certain that there is an infection present, if you’re not certain if you have COVID, definitely stay away from people who don’t have a normal immune system or who are very elderly or who have other underlying diseases.”
He added that if you’re one of the rare cases who tests positive but have no symptoms, you should go by your test results.
“If you test positive for COVID, it means you’re shedding virus,” he said. “So if you have a positive test, I would stay inside and isolate.”
Long COVID and prevention
At this point, most people have developed a base level of immunity to COVID-19, which means a decrease in how long and how sick you become. But there’s another risk to worry about — long COVID, the symptoms of which can, in some cases, last for years.
“Long COVID is still a risk of any COVID infection,” Fishman said. “It’s difficult to quantify the risk. And we don’t know whether the risk changes or is different for these different strains that we see.”
What we do know, he added, is that many people do get better from long COVID — eventually.
“It can take six months or nine months or sometimes longer, but people do recover from long COVID,” Fishman said.
One way of decreasing your risk of long COVID, he added, is to take Paxlovid.
Better yet, is to avoid getting sick altogether — and for that, recommendations remain the same as always.
“My take-home PSA would be stay home if you’re sick, clean your hands, cover your cough,” Fishman said. “And while we are still experiencing peak activity, consider masking in crowded environments. And I think the riskiest in our area now is probably public transportation. When you’re outside in the open, it’s safe; there’s good air circulation. If you’re in a contained, crowded environment, the risk of acquiring the infection is higher.”

Get daily updates from WHYY News!
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.






![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)


