As FDA requires national breast density notification, Delaware Valley women say more counseling is needed
As of September 10, all mammogram centers and providers are required to inform patients if they have dense breast tissue, which can make screening more difficult.
Listen 5:56
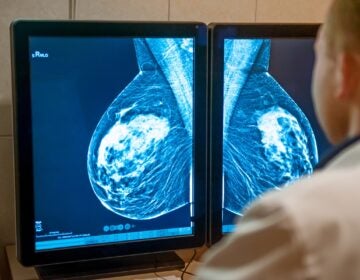
Staff of Penn Medicine’s mobile mammography unit demonstrate how patients receive a mammogram on Oct. 22, 2021 in Philadelphia. (Kimberly Paynter/WHYY)
From Philly and the Pa. suburbs to South Jersey and Delaware, what would you like WHYY News to cover? Let us know!
Valerie Marlett started getting annual mammograms last year when she turned 40. Her first screening report told her she had dense breast tissue, but it didn’t seem like an immediate cause for alarm.
“It was my first mammogram,” she said, “and, you know, my OB-GYN is not concerned. Nobody’s concerned.”
The report explained that dense breast tissue can make it harder for a mammogram to detect cancer, especially in early stages, so additional screening might be recommended. Dense tissue is also independently associated with a higher risk for cancer.
To Marlett, who lives in Delaware, it was information with no clear instructions on what to do next.
“I really didn’t know half of the words that were in the report,” she said. “I just picked up on, OK, everything came back normal. I just went on with life.”
But when Marlett had a mammogram this year, it came back inconclusive. Her doctor recommended a second mammogram, which led to a breast ultrasound and a biopsy. Marlett was diagnosed with breast cancer this summer.
She now wonders if the cancer could have been found earlier, after her first-ever mammogram last year, had she asked for additional screenings like an ultrasound or MRI.
“I think I wish that there were more people in health care that maybe pushed it and explained it to me a little bit more the first time around,” Marlett said.
About one in eight women will get diagnosed with breast cancer in her lifetime, national data show. And breast density can play a role in someone’s cancer risk and their ability to get accurate screening tests.
As of September 10, the U.S. Food and Drug Administration now requires all mammography centers across the country to notify women if they have dense breasts and about additional screening options like breast ultrasounds and MRIs.
Some states like Delaware, New Jersey and Pennsylvania have had breast density notification laws for years, but local women said the information is insufficient. They say more consistent education and counseling are needed to make the process less stressful for patients and allow them to make fully informed decisions about their health care.
“It feels a little disjointed,” said Garden Logan, 53, of Haddonfield, New Jersey. “I wish it was more of a cohesive back-and-forth communication and understanding of options. What can I do to advocate for myself and make sure I’m not leaving any stone unturned with this situation?”
Mammograms are still the gold standard of screening tests for breast cancer. National recommendations say most women should get screened every year beginning at age 40. Women with a family history may start earlier in their 30s.
However, radiologist Dr. Claire Streibert, site chief of breast imaging at Fox Chase Cancer Center at Temple Health, said dense tissue appears white on imaging. So does cancer.
“I’ve definitely seen those cases where those women then have gotten an additional breast ultrasound, and we’ve found a small cancer there that we would have never seen on her mammogram until it distorted the breast tissue,” Streibert said.
Research on the effects of breast density notifications on cancer outcomes is still limited, but studies do show that ultrasounds and MRIs can better detect breast cancer in patients with dense tissue, which may mean less invasive treatment down the road.
Streibert said not all women who have dense breasts will need additional screening ultrasounds or MRIs. They’re mostly recommended for patients with moderately or extremely dense tissue and other risk factors, like a family history of breast cancer or certain cancer genetic mutations.
Therefore, a person’s cancer risk and screening recommendations may be very individualized, but the initial notifications go out to all women with dense breast tissue. Jessica Scott, 49, of Philadelphia, said that can be confusing, especially when there’s no clear guidance, or conflicting guidance, from health providers on what to do next.
“So that in and of itself, as a woman who knows nothing about this, is confusing,” Scott said. “I trust the experts, and if the experts aren’t quite sure, that doesn’t feel super great.”
While breast ultrasounds and MRIs can better detect cancer in dense breasts, they can also lead to false positives. It means women may get biopsy procedures for things that end up being non-cancerous tumors or cysts.
Scott, who has experienced her own false alarm, said the anxiety and panic this can cause may put some women off from scheduling their next yearly screening if they don’t get the right information and medical guidance throughout the process.
“I could imagine anyone who has any type of aversion to the doctor would not even go knowing that they’re opening themselves up to a whole process that isn’t super clear,” she said.
Dr. Peter Gearhart, an OB-GYN at Pennsylvania Hospital in Philadelphia, fields many calls from concerned patients who have gotten dense breast notification letters and want to know what to do.
He said providers are still playing catch up to newer research and data about breast density and screening outcomes.
“Part of what patients are experiencing over the last five years or so is this evolution of knowledge within the field about dense breasts,” Gearhart said. “Maybe 10 years ago, we didn’t know as much about it. Now that we know more about it, we’re able to provide better counseling.”
Gearhart said health organizations are trying to figure out how to devote more resources to patient education and guidance about breast density to make it a less confusing and stressful experience.
Another barrier that can get in the way of receiving appropriate follow-up care is cost. Additional screening tests can be expensive, and coverage varies greatly depending on where a woman lives, what kind of health insurance plan she has and even where she works.
Laurie Scofield founded DENSE NJ, an advocacy organization, after her own experience with dense breasts and a later-stage diagnosis of cancer. She and other advocates with the national DenseBreast-info, Inc. have led efforts to pass notification laws and are now focused on insurance coverage mandates.
“[Women] are told, ‘Your insurance isn’t going to cover it’ or ‘You can go, but your deductible, it’s going to be $2,000 dollars. Whatever your deductible is, you’re going to have to pay that.’ And there are a number of women who cannot afford that.”
States like Pennsylvania have only recently passed laws requiring insurance coverage for additional screening for women who have dense breasts and are considered “high risk” for cancer. But mandated coverage does not apply to all companies and businesses that offer health care plans to their employees.
“We have to make it affordable,” Scofield said. “We have to allow women to get the detection that they need.”
Quick facts about dense breasts and cancer screening
- Dense breast tissue is common. An estimated 50% of women in the United States who get mammograms at 40 and older have this.
- Only radiologists who use mammograms and other screening tests can detect dense breast tissue. It cannot be felt during a self-exam or diagnosed by a primary care provider or OB-GYN during a clinical exam.
- The size and shape of breasts do not predict breast density. It is more often associated with people who are younger in age, hormone production and women taking menopausal hormone therapy.
- Breast density falls into four categories: entirely fatty; scattered fibroglandular; heterogeneously dense; and extremely dense. Patients in the latter two categories receive
- dense notifications after mammograms.
- Although dense breast tissue is an independent risk factor for breast cancer, women with dense breasts who develop cancer are not at a higher risk of dying compared to other women with cancer who do not have dense breasts.
Source: The National Cancer Institute

Get daily updates from WHYY News!
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.