Avoid processed red meat, wildfire smoke and more: 4 takeaways from the Alzheimer’s Association International Conference in Philly
Here’s what to know about the latest research on Alzheimer’s risk factors and treatments.
Listen 1:03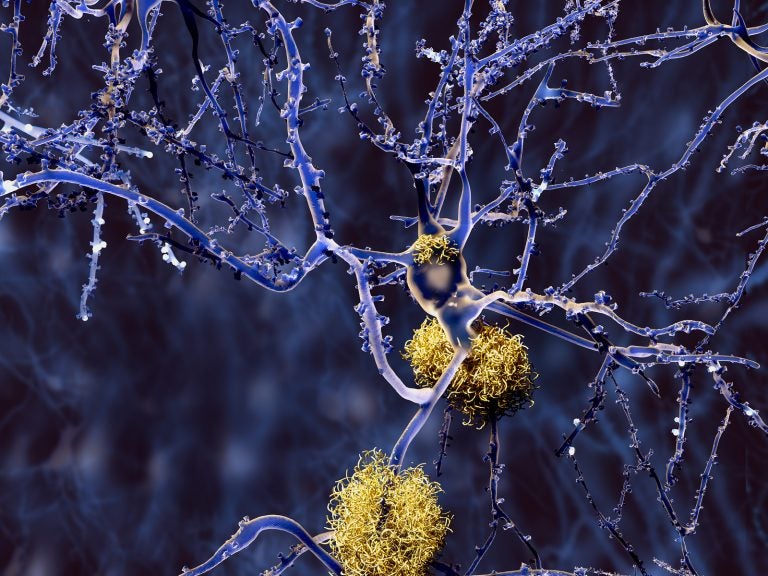
Amyloid plaques accumulate outside neurons. Amyloid plaques are characteristic features of Alzheimer's disease. (Bigstock/animaxx3d)
From Philly and the Pa. suburbs to South Jersey and Delaware, what would you like WHYY News to cover? Let us know!
More than 10,000 dementia researchers and clinicians from around the world have gathered in Philadelphia for the annual Alzheimer’s Association International Conference, or AAIC. Over five days — featuring more than 150 scientific sessions, 800 podium presentations and more than 4,000 posters — experts will discuss the biggest advancements, discoveries and questions facing the field.
“The breadth and the depth of research that we see at AAIC is really unparalleled,” said Claire Sexton, the senior director of scientific programs and outreach at the Alzheimer’s Association. “It’s a key part of the dementia science calendar because it offers sessions from basic science biomarkers through to drug development, then through to public health and dementia care. So really every single aspect of Alzheimer’s and dementia science is represented here at AAIC.”
Here are some key takeaways from the conference:
1. A blood test can now catch 90% of early dementia cases
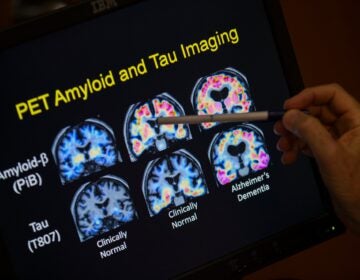
For years, clinicians have relied on a battery of often expensive and invasive tests to diagnose Alzheimer’s disease, ranging from neurological exams to brain scans to spinal taps.
But a new study presented at AAIC confirms that a blood test can now accurately diagnose Alzheimer’s 90% of the time, compared with 73% for dementia specialists and 61%for primary care physicians.
The test measures levels of p-tau217, a protein that builds up in the brains of people with Alzheimer’s.
“This has been something which has been really a key area of focus and garnered a lot of excitement in recent years,” Sexton said, “because [blood tests would] be cheaper, could be more accessible than other ways of measuring pathology.”
2. Processed red meat raises the risk of dementia
Here’s another reason to cut back on bacon, bologna and hot dogs: a study released Wednesday finds that processed red meat increases the risk of dementia.
These findings have been a long time coming. The study followed 130,000 people for up to 43 years and found that as little as two servings of processed red meat per week raised dementia risk by 14%, compared with those who eat less than three servings a month.
But there is some good news: the study didn’t find a significant association between dementia and unprocessed red meat, like steak, pork chops and hamburger. It also found that replacing one serving of processed red meat per day with nuts or legumes lowered dementia risk by 20%.
3. Wildfire smoke worse than other forms of air pollution
A study presented on July 29 shows that wildfire smoke increases the risk of dementia more than other forms of PM2.5 (or fine particulate matter) air pollution, including that produced by cars and factories — even with less exposure.
Researchers reviewed 10 years’ worth of health records belonging to southern Californians age 60 and older, none of whom were diagnosed with dementia at the start of the study. They found that every 1 microgram increase of PM2.5 wildfire smoke pollution per cubic meter of air increased the risk of dementia by 21% over three years, compared with just 3% for every 3 microgram increase of non-wildfire PM2.5 pollution.
The solution? Staying inside during wildfires, wearing N95 masks when you need to go out and updating your home air filtration system if possible.
4. Updates on the promise of Alzheimer’s drugs
Liraglutide — a medication in the same class as Ozempic that is used to treat type 2 diabetes and obesity — could help slow the progression of Alzheimer’s disease by protecting the brain.
That’s according to data drawn from a phase-2 clinical trial presented at AAIC. Researchers found that patients who received injections of liraglutide, known on the market as Victoza and Saxenda, had an 18% slower decline in cognitive function over the course of a year compared to those given a placebo. They also experienced 50% less shrinking in parts of the brain that control memory, learning, language and decision-making.
Conference attendees also received an update on lecanemab, sold under the brand name Leqembi, a monoclonal antibody drug approved last year by the FDA for the treatment of early-stage Alzheimer’s.
Eisai and Biogen, the companies that make lecanemab, reported that the drug offered continuous benefits over three years of use among 50% of patients in the early stages of Alzheimer’s.
Lecanemab has been shown to moderately slow cognitive decline among those in the early stages of Alzheimer’s, but has been greeted with caution due to the risk of serious side effects, including swelling and bleeding in the brain.
For further information, clinicians and members of the public can register for “AAIC for All,” a free webinar on Aug. 1 that will offer highlights of the new research presented at this year’s AAIC.

Get daily updates from WHYY News!
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.