Penn researchers find killing dormant, ‘sleeper’ breast cancer cells may prevent recurrence
New results from a clinical trial show that existing drugs can successfully kill dormant breast cancer cells, thereby reducing lifetime risk of recurrence.
Listen 1:32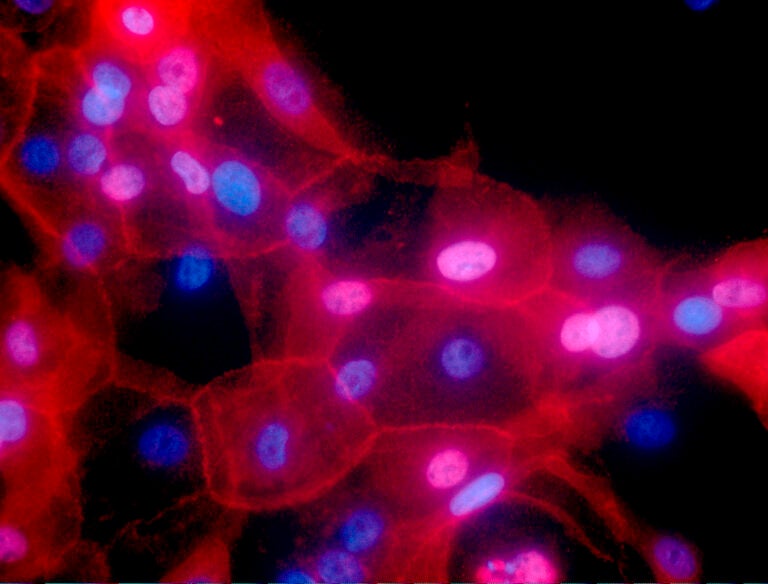
FILE - This undated fluorescence-colored microscope image made available by the National Institutes of Health in September 2016 shows a culture of human breast cancer cells. (Ewa Krawczyk/National Cancer Institute via AP)
From Philly and the Pa. suburbs to South Jersey and Delaware, what would you like WHYY News to cover? Let us know!
Researchers at Penn Medicine say they’ve found a way to test for dormant breast cancer cells in survivors and successfully eliminate those cells before they become active in the body, effectively preventing the disease from returning.
Experts published their findings Sept. 2 in the medical journal Nature Medicine, and are now testing the prevention strategy in ongoing large-scale clinical trials involving hundreds of breast cancer survivors around the country.
“It would dramatically change things for every single breast cancer patient,” said Dr. Angela DeMichele, co-leader of the Breast Cancer Program at the University of Pennsylvania’s Abramson Cancer Center. “Because for those in whom we find cells, we can do something. And being able to tell a woman, ‘You don’t have any of these cells,’ would free her from that worry.”
For the more than 300,000 women who get diagnosed with breast cancer every year in the United States, the test could eliminate the uncertainty that usually comes after the initial disease is treated.
On average, experts say the cancer will come back in about 30% of cases, oftentimes in an advanced stage or incurable.
“And the problem is that we don’t know who that woman is, whose cancer is going to come back and who truly will be cured,” DeMichele said.
Doctors and health providers can generally calculate a person’s individual risk for breast cancer recurrence, but it still requires a lot of guesswork, bringing anxiety and fear for survivors.
“If someone says, ‘Hey, you have a 40% chance that your cancer’s going to come back,’ what does a woman, or a man, do with that information?” DeMichele asked. “It’s really scary.”
Testing for cancer ‘sleeper cells’ that lay dormant
Studying dormant cancer cells and their role in cancer recurrence is a growing area of research.
Dr. Lewis Chodosh, an endocrinologist and chair of the Department of Cancer Biology at University of Pennsylvania Perelman School of Medicine, has dedicated much of the last two decades to better understanding these types of cells.
He first looked at breast cancer in mice and how the cancer would return in some of the surviving animals.
“And it dawned on us that, well, if the cancers come back, that must mean there’s still cells in the body even though we can’t find them, if you can’t feel any tumor in the mouse,” Chodosh said.
These leftover cells, scattered in the body, are microscopic and not detected with standard medical tests, he said. And they’re dormant, meaning they’re not growing and multiplying as they stay hidden for years or even decades, until they suddenly “wake up.”
“Like dandelion seeds in the wind, they wind up in your lawn, you can’t see them, but they’re there,” Chodosh said. “And someday when it rains, one of those is going to sprout and then you’re going to see it and it’s too late.”
After learning how the dormant cells survive for so long, researchers tested ways to kill those cells, or at least significantly reduce the number of them, before they ever became active.
They found success with two existing oral drugs: hydroxychloroquine, which is typically used to treat autoimmune diseases, and everolimus, which is used to treat some kidney and breast cancers alongside other therapies.
Penn researchers then took this strategy and applied it to humans.
Breast cancer survivors take action in preventing recurrence
Jamie LaScala was just 40 years old when she was diagnosed with Stage 3 inflammatory breast cancer, a rare and aggressive form of the disease. It was caught in 2015 during her first mammogram.
Chemotherapy, radiation and surgery led to a successful recovery, but LaScala, who lives with her family in Wilmington, said a part of her always worried if the cancer might one day come back.
She then heard about the clinical trial at Penn Medicine, where researchers were testing breast cancer survivors for dormant cancer cells in their bone marrow, which if present, would indicate a higher chance of recurrence someday.
“And I said, ‘I want to be part of the trial. I want to know if I have these,’” LaScala said.

LaScala enrolled in the phase 2 CLEVER trial, which started in 2017 and ran throughout the COVID-19 pandemic.
Her first two bone marrow tests were negative for the dormant cells, but the third test was positive. She started taking six cycles of medication to eradicate the cells.
The trial, which enrolled 51 patients from the Greater Philadelphia area and across the U.S., found that the medication treatments cleared dormant cells from 80% of participants. After seven years of follow-up study, only two people have since relapsed and had their breast cancer return.
LaScala, now 50, has remained cancer-free for nearly a decade.
“If by following us they can glean any kind of insight into who has more potential to recur versus less, I think there is that element of wanting to help get answers to this,” she said.
Reducing anxiety and providing reassurance for patients
The team at Penn is currently enrolling patients in two ongoing, large-scale studies that could help support their findings. Trial sites are located across the country, including at the University of Pennsylvania in Philadelphia.
The ultimate goal, Chodosh said, is to not only identify and treat those who are at a higher risk of recurrence, but to be able to offer reassurance to survivors who don’t have dormant cells.
“The goal would be to get a test that’s so good that, if you’re negative with this test, you could confidently say your risk of recurring is extremely low over the course of your lifetime,” he said. “That would have such a big benefit.”
Researchers are also following breast cancer survivors who don’t ever test positive for dormant cancer cells in order to compare their long-term survival outcomes to those who get treated for sleeper cells.
Some clinicians and experts were worried about whether participation in these kinds of trials would cause more distress in survivors, DeMichele said. But her team studied that, too, and found it to be the opposite.
“Regardless of the answer, whether the patient found out they were positive or negative, overall their anxiety went down,” she said. “And we think it’s because, and what patients tell us is, ‘Look, at least I’m doing something.’ It was the not doing something, not knowing, that was so anxiety-provoking.”
Over the years, LaScala has become more involved in research efforts and now serves as a patient advocate on research boards at Penn, where she can help shape studies and participant guidelines.
Among breast cancer survivors, she said there has always been passion and an eagerness for advancing testing and treatment options for everyone — survivors, people actively battling disease and those who may one day get a diagnosis.
“It’s so energizing,” LaScala said. “To be around the research and to be able to participate … it’s incredible.”

Get daily updates from WHYY News!
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.