In race for COVID-19 vaccinations, older residents in rural Pa. face tough obstacles
Despite being among the most at risk, some lack transportation, access to chain pharmacies, and internet connections to get vaccine appointments.
(Fred Adams for Spotlight PA)
Spotlight PA is an independent, non-partisan newsroom powered by The Philadelphia Inquirer in partnership with PennLive/The Patriot-News, TribLIVE/Pittsburgh Tribune-Review, and WITF Public Media. Sign up for our free newsletters.
Robert Keen figured his year of dodging the coronavirus was over.
At 84, the retired ambulance driver — who still works with his local fire department — is among the most at-risk from the disease, and thus was given top priority to get the vaccine. So he called up his doctor last month to schedule an appointment.
He was told he would have to wait until April.
Keen lives in Forksville, a borough in Sullivan County about 60 miles west of Wilkes-Barre in the northeast. The county has a population of about 6,000 and does not have a hospital. There’s one stoplight, hundreds of acres of forests and state game lands, and one public school district.
The pharmacy and medical center are too small to take on the work of administering coronavirus vaccines. Most residents get their health care at hospitals or doctor’s offices at least an hour away in neighboring counties.
Scheduling a vaccine appointment in Pennsylvania is already a competitive process exacerbated by a short supply and patchwork online scheduling systems.
But older residents — who are supposed to be among the first in line — in rural areas face more obstacles. They live far away from major chain pharmacies like CVS and RiteAid, and may not have internet or a means of transportation. Three rural counties — Forest, Fulton, and Sullivan — do not have major chain pharmacies that are participating in state and federal vaccine distribution programs, according to an analysis by Keith Mueller, director of the RUPRI Center for Rural Health Policy Analysis at the University of Iowa.
Rural counties also tend to have a larger share of older residents. About 17% of Pennsylvania’s 12.8 million residents are older than 65, Census data show. In many rural counties, older residents make up about 20% of the population.
“We’ve known that our population is very heavy on 65 and older,” Sullivan County Commissioner Brian Hoffman said. “We don’t have a large medical provider or a hospital … those two elements drove much of our preplanning.”
In Venango County in the northwest, Commissioner Albert Abramovic said he was worried about connecting residents who don’t have internet or cell phone service with appointments. About 21% of the county’s 50,000 residents are older than 65, according to Census data, and 22% of households don’t have internet access.
Abramovic said he’s heard of people waking up at 5 a.m. to log on to pharmacy scheduling websites or signing up multiple times to improve their chances of landing a spot.
In Juniata County, 19% of the population is older than 65 and a quarter of households do not have internet access. Some older residents live alone, on old family farms, said Alice Gray, one of the county’s commissioners.
“Many of our older folks, they aren’t computer savvy,” Gray said. “They don’t use computers. So if the only way they have is to schedule an appointment via the internet, I don’t know if they know how to do that.”
A Weis grocery store and a health clinic in Mifflintown are the only sites offering vaccines in Juniata, according to state data. From the farthest reaches of the long, narrow county, getting there could be a 40-minute drive, Gray said.

‘Hodgepodge’
In a statement in late January, Sen. Lindsey Williams (D., Allegheny) called for a system to alert residents when it’s their turn to sign up, along with stronger partnerships with local, independent pharmacies to reach residents, like Keen, who don’t have access to corporate chains.
“After more than 10 months of the uncertainty and hardships that this pandemic has brought us, Pennsylvanians are confused and anxious to receive a vaccine, and they deserve clearer communication and more concrete answers,” Williams said.
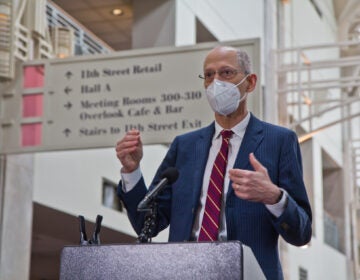
Following a January hearing featuring health care providers distributing vaccines in rural areas and state health officials, Sen. Gene Yaw (R., Lycoming) described the state’s distribution system as a “hodgepodge” and criticized the health department for poor planning and communication.
“The bottom line is we need more vaccine,” said Yaw, who is also chair of the Center for Rural Pennsylvania, a legislative agency focused on Pennsylvania’s rural communities.
“The distribution system we have out there … I think we have to live with it,” Yaw said. “It’s too far along to go back and make a wholesale change at this point.”
As of Feb. 4, more than 880,000 people have received at least one dose of a coronavirus vaccine, state data show, but about four million people are eligible to be vaccinated as part of the state’s Phase 1A, necessitating about 8 million doses.
Residents who qualify now need more and better communication — like ads or explainers in print media — that don’t require the internet or a computer to access, Yaw said.
Some local governments have raised questions about whether they can get help from the National Guard. Acting Health Secretary Alison Beam said Wednesday its units are currently focused on responding to outbreaks in the state’s long-term care facilities, but that the state is working to launch community clinics.
One recent clinic was in Pike County, in the northeast, and another in Sullivan, where Keen lives. Both were chosen by the state because those counties lack health care infrastructure. The clinics also created an opportunity to address other distribution challenges, like how to get vaccines to a large population of older residents and those without transportation.
In Sullivan, about 27% of residents are older than 65, and 22% don’t have internet access.
Officials in other counties are also preparing to launch local mass vaccination clinics.
Throughout January, Kevin Boozel, a commissioner in Butler County in southwest Pennsylvania, said his office fielded as many as 70 calls and emails a day from residents frustrated that they don’t have information about where to get a vaccine.
“I think people believe that we as county commissioners are holding back the vaccine,” said Boozel, who is also president of the County Commissioners Association of Pennsylvania.
Many counties have worked with their local emergency service departments to put plans together for community vaccination clinics, and they’re brainstorming ways to reach people living in public housing and to use plans developed during previous emergencies, like the H1N1 flu outbreak, Boozel said.
“We stand ready to help as we continue to work through this pandemic,” he said.
None of their plans can be enacted until the state tells counties how many doses they will receive, where they’ll go, and when those shipments will arrive, he said.
Warren General Hospital, an 85-bed community hospital in Warren County, has been vaccinating about 600 to 1,000 people per week, Richard Allen, hospital CEO, said during a state House health committee hearing Wednesday.
They’re not equipped to handle a larger volume of people while still running the hospital. As more become eligible to receive the vaccine, they will need help, Allen said.
“In the face of these uncharted pandemic waters,” Allen said, there is “a void in terms of coordinated direction, authority, and resources.”
Primary Health Network, which serves residents in rural counties throughout the state, recently acquired a mobile health unit that will be used for both coronavirus testing and vaccines, said Dr. George Garrow, chief medical officer for the network.
But even as the system gears up to vaccinate people who aren’t able to reach a vaccination site, it has had to close offices — which are sometimes as small as three people — if staff are exposed to the coronavirus, Garrow said during a January hearing with the Center for Rural Pennsylvania.
“As this situation progresses, I do see it necessary to engage with the National Guard to assist in vaccinating mass quantities of communities,” he said.

A model for the state?
Mobilizing vaccination efforts in rural areas takes more than just someone to give the shot.
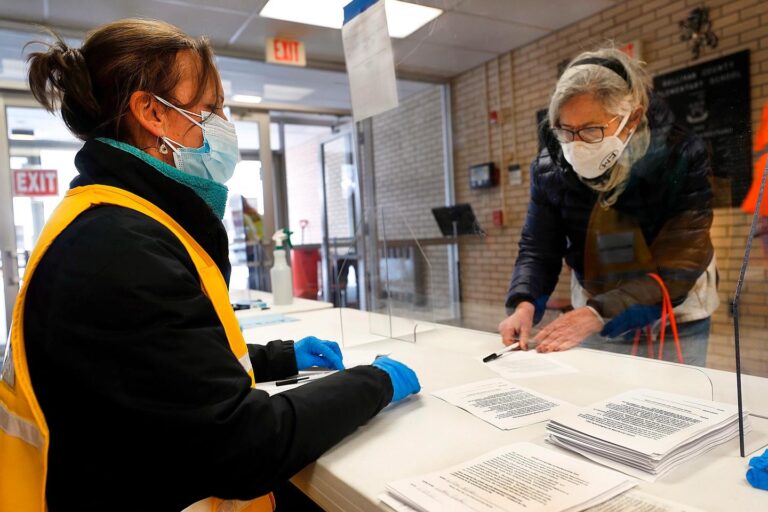
After it got word from the state that a clinic could be held in Sullivan County, local officials decided it should be held at the Sullivan Elementary School in Laporte — a familiar, central location that often doubles as a space for community events.
Public transportation is limited: The county got its first public bus route in October, and getting around requires “a car, or a relative who has one,” Commissioner Darlene Fenton said.
The plan was to vaccinate 500 eligible people on Jan. 29 and Jan. 30.
Information was posted on the local government website earlier that week, said Hoffman, the commissioner. By the time the local weekly newspaper, The Sullivan Review, ran a summary outlining details of the event in its Jan. 27 edition, all of the appointments had been filled.
“The demand for vaccines was definitely more than our available supply,” he said.
The local Area Agency on Aging, which works with the county’s older residents to connect them with personal care resources, helped them register. Other eligible people heard through their local emergency medical services and fire department, including Keen.
Five older residents who received vaccines Friday relied on a special service provided by the local tri-county transit system to make it to their appointments. Four are already scheduled to use the service when they return for their second dose in late February.
It took a team of at least 54 people — including local volunteers in color-coded vests to check in residents, medical workers, county employees, and state health department staff — to keep the clinic running, according to figures provided by Sullivan officials.
Inside, however, it felt more like a gathering than a vaccination site, with laughter and neighbors catching up with each other for the first time in months.
“We’re a small county,” Hoffman said. “So a lot of people already know each other and already worked together on other things.”
Maryanne Karpovich, an 85-year-old from Dushore, has a pulmonary disease and a pacemaker — “two strikes against me,” she said. Before scheduling with the clinic, she tried to track an appointment down elsewhere, but was told she’d have to wait weeks.
“You won’t be as afraid,” Karpovich said after receiving her shot. “But you still have to wear the mask.”
After being told by his doctor he’d have to wait until April, Keen received his first dose of the Moderna vaccine Jan. 29.
“I feel great,” he said afterward.


Get daily updates from WHYY News!
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.




![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)



