‘A war against ourselves’: Why Pa. and N.J. are preparing now for a delta variant surge
New Jersey and Pennsylvania have been shielded from the delta outbreaks seen in other parts of the country. That trend line is changing.
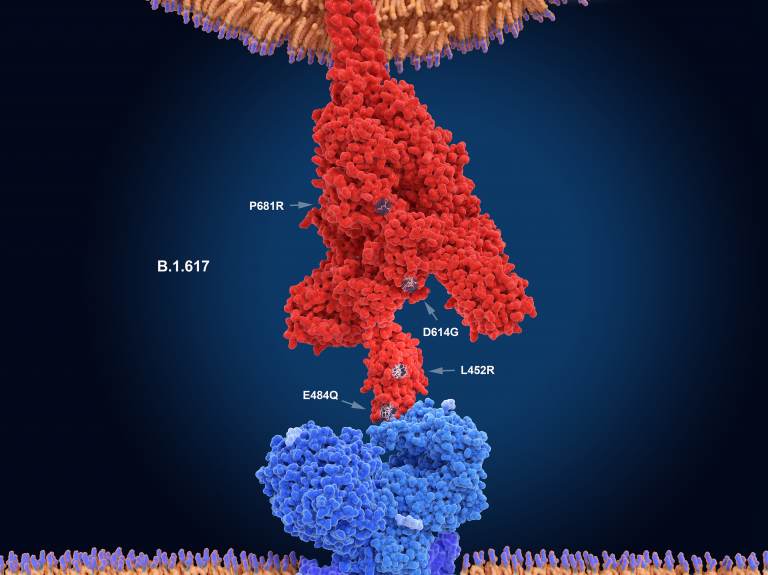
The numerals in this illustration show the main mutation sites of the delta variant of the coronavirus, which is likely the most contagious version. Here, the virus's spike protein (red) binds to a receptor on a human cell (blue). (Juan Gaertner/Science Source)
Ask us about COVID-19: What questions do you have about the coronavirus and vaccines?
Both Pennsylvania and New Jersey have so far been shielded from the worst outbreaks of the delta variant, unlike places like Louisiana and Florida, which have seen rampant spread and flooded hospitals. But experts, and new data, indicate the calm is unlikely to last long.
The lessened spread locally, at least thus far, likely owes to generally higher vaccination rates in the northeastern United States and other complex factors, ranging from varying population density to tourism. Even so, Dr. Esther Chernak, director of the Center for Public Health Readiness and Communication at Drexel University, says rates are virtually guaranteed to continue to increase locally.
“It’s just beginning to be experienced in this area. I think we’re on the uptick here,” she said. “The issue with the delta variant is that it’s going to find the most vulnerable part of our community.”
Both Pennsylvania and New Jersey are below the national case rate of 26 infections per 100,000 residents. However, there is also a noticeable disparity between the two states — with New Jersey seeing more cases thus far than the Keystone State, despite a higher vaccination rate.
Although about 66% of residents in both states have received at least one vaccine shot, New Jersey has a higher portion of its population fully vaccinated at 59%, compared to 53% in Pennsylvania. Nevertheless, New Jersey is seeing new infections at a higher rate: about 11 per 100,000 residents, compared to 8 per 100,000 in Pennsylvania. The cases add up to a triple-digit case increase in both states over the last two weeks. Although death rates have generally lagged infections and, nationally, elderly people have been vaccinated at higher rates, the increased contagiousness of the delta variant means that mass outbreaks would still be deadly.
Why? Chernak credited a combination of factors — possibly even the Garden States’ famed beach tourism.
“New Jersey has more tourism, and that means more people doing things that promote disease transmission: people traveling in from other states, people importing the virus,” she said. “Pennsylvania is very different. You do have a couple of large metro areas, but you also have lots of rural areas.”
Dr. Mark Roberts, director of the Public Health Dynamics Lab at the University of Pittsburgh, said more sparsely populated areas might help slow the spread of the virus, but would not act as a shield forever.
“New Jersey, in general, is a denser state. Density is important for a disease that relies on proximity to transmit,” he said. “But you’re still seeing it everywhere, across New York, Maryland, Ohio, are all seeing it.”
In fact, some areas in Pennsylvania already seeing the worst rates of infection are comparatively rural.
Places like Wyoming or Lawrence County are currently seeing rates as bad as some North Jersey suburbs of New York City or cities like Philadelphia — with averages ranging from 8 to 12 cases per 100,000 residents. The hospital with the highest rate of COVID-related hospitalizations in either state at the moment is in Danville, Pennsylvania, which has seen dozens of severe cases despite being located in a county with just over 18,000 residents.
Some of the counties serviced by Danville had below-average vaccination rates, while others were above average. Still, Dr. Alison Brodginski, director of infectious diseases for Geisinger Medical Center in Danville blamed the overall slowing rate of vaccination for the outbreak in Danville.
“The great news is that we have not had anyone in our intensive care unit, and we have not had any deaths in any patient that has been fully vaccinated,” Dr. Brodginski told WNEP this week. “Unfortunately, we’re not seeing that demand [for vaccinations] that we were seeing months ago, even weeks ago.”
While research shows it is possible in rare cases for vaccinated individuals to contract the virus — so-called breakthrough cases — and spread it, Roberts said unvaccinated people were the primary drivers of the delta variant.
Rural areas have generally seen lower rates of vaccination than urban areas, but in the suburban and urban areas experiencing spread, there are still millions of unvaccinated people able to spread the virus.
“County by county, it does vary,” he said. “But here in Pittsburgh and Allegheny County, for example, virtually all COVID-19 patients have been unvaccinated … and nationally you’ve seen more cases where vaccination rates were low.”
With 53% of all residents fully vaccinated, Pennsylvania is only slightly ahead of some states hit hard by delta — like Florida, which has fully vaccinated 49% of all residents.
Dr. Paul A. Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, urged policymakers to act sooner than later, with the creeping onset of colder weather and traditional cold and flu season.
“Obviously, the delta variant is much more contagious, so it’s been able to seek out and hurt those who are the most vulnerable. And it’s still just the summer,” he said. “You’re about to have unvaccinated children coming back to school, gathering together during the fall and winter.”
There were still steps that could be taken, he said, such as instituting vaccine mandates. While political leaders have generally avoided serious discussion of such policies, Offit noted that vaccine mandates have been used for decades, particularly in schools.
In 2019, when flagging vaccination rates led to measles and whooping cough outbreaks in Southern California, doctor and State Sen. Richard Pan helped push through strict controls on vaccine exemptions for school children, eventually bringing rates close to 100% among kindergarteners.
Still, figures like Pan were assaulted by anti-vaccination activists and such measures today remain politically unpalatable. While some link the current surge of anti-vaccination sentiment to far-right politics, even in Democratic strongholds like Philadelphia city leaders have balked at mandating vaccination for city workers. Pennsylvania Gov. Tom Wolf has indicated that even mitigation efforts like mask mandates were highly unlikely to return en masse.
“We’ve made it political. When has that ever happened before? Imagine if that happened with smallpox or polio,” said Offit. “The war here is supposed to be against the virus. But it’s become a war against ourselves.”

Subscribe to PlanPhilly
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.




![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)



