From ’80s to now: Waves of investment in drug treatment can help, hurt patients
Listen
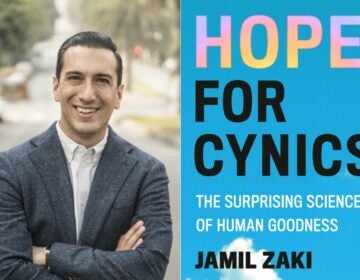
David Dorschu and Deni Carise with Recovery Centers of America standing in a room at the Lighthouse at Mays Landing, a treatment center the company flipped for $1.25 million last year. (Laura Benshoff/WHYY)
Just as the clothes we wear and the restaurants we visit follow trends, the illicit drugs we ingest cycle in and out of fashion.
In the 1980s, shoulder pads were in, the USSR was still together, and the drug “epidemic” was fueled by cocaine along with its cheaper derivative, crack.
At the same time, growing public awareness of addiction — and recovery — created a whirlwind of investment in treatment services. In 1982, former first lady Betty Ford’s admission that she abused prescription pills and alcohol showed that not even the first family is immune.
“The ’80s really became a time when celebrities, athletes kind of jumped on this bandwagon that it was actually kind of cool to be in recovery,” said Doug Tieman, CEO of Caron Treatment Centers, a large nonprofit provider founded in Berks County.
Demand for services, diminishing stigma and relatively loose insurance rules triggered a flood of investment from Wall Street into recovery services in the late 1980s as a part of a larger push for health care consolidation.
As someone who’s been in the treatment business for a long time, Tieman has hit the lecture circuit with a cautionary tale, aimed at investors. “We had people go to jail in the ’90s for insurance fraud, Medicaid fraud,” he tells them
Another casualty was the public’s trust in treatment providers.
In the 1990s, fraud led to a clampdown on insurance coverage for treatment, making investing in treatment centers less profitable. But trying to control spending wound up hurting clients, who lost access to subsidized care.
The present
Fast forward to 2008, when a new day was dawning on mental health policy in the U.S. That year, President George W. Bush signed the Mental Health Parity and Addiction Equity Act into law, requiring large group insurance plans to cover mental health in the same way as other medical conditions.
Two years later, President Barack Obama signed the Affordable Care Act, pulling more addiction services under the umbrella of insurance.
That set the stage for an investment frenzy at an even higher pitch than before.
“I don’t think that the public and the investment industry has seen this kind of opportunity to produce income from treating addiction ever before,” said Marvin Ventrell, executive director of the National Association of Addiction Treatment Providers.
Outpatient centers, detoxes and drug-testing labs are being purchased, bundled together and sold for vast sums of money.
In 2005, Bain Capital bought the largest addiction-service provider in the country, CRC Health Group, for $720 million. In 2014, it turned around and sold it to another company, Acadia Health, for $1.18 billion.
Money magnifies strengths and weaknesses
Vast sums of money act as an accelerant for both good and bad ideas. In the addiction-treatment field, it’s also lured new players onto the scene.
Recovery Centers of America is the brainchild of real estate developer Brian O’Neill, based in King of Prussia. The company is backed by more than $330 million from Deerfield Management Company, a hedge fund.
About $1.25 million of the company’s resources went into buying and sprucing up Lighthouse Recovery in Mays Landing, a 53-bed facility near the New Jersey Shore.
In the new Lighthouse, gone are the heavy brown couches. Instead, sunlight streams in through big windows in the common areas, decorated in pale blues and white like a tasteful beach house.
Underpinning the plush surroundings is a mantra that treatment should be inviting.
“We offer yoga twice a week for every patient in small groups, exercise classes twice a week … we also have meditation,” said Deni Carise, chief clinical officer for Recovery Centers of America.
In addition to providing hotel-like amenities, Recovery Centers of America tweaked the residential treatment model to reflect what insurance will actually cover.
“The average stay here is 12 days, between detox and residential,” said Lighthouse’s director of operations, Michael Desrosier. Traditional residential treatment lasts 30 to 90 days, with the prevailing wisdom holding that longer stays correlate more with success — although medication and other factors make a significant difference in the case of opioid addiction.
By contrast, insurance often covers less than two weeks, so Recovery Centers of America slots its clients into a web of outpatient services to try to keep them on the road to recovery.
In addition to trying novel treatment models, places with big backers like RCA can devote a larger part of their budget to marketing. To compete, less scrupulous providers are playing dirty to get clients.
Patient brokering, $1,200 pee tests
Overbilling and unnecessary testing are just two items on a menu of unethical techniques that have spread, according to Tieman of Caron Treatment Centers.
Alice LaRocca has encountered them first hand.
“My God, the things you find,” she said with a laugh, sitting in her home office in Sicklerville, New Jersey, about 20 minutes from Philadelphia.
The mother of two estimates her older son, Shane, has sought treatment for opioid addiction 15 times over the last 10 years, mostly in South Florida.
Treatment was usually a good experience, but, afterward, Shane wound in more than one sober-living home or intensive outpatient facility that took advantage of him — and his health insurance.
“One place, it looked like he was doing great. And then, three weeks later, I find out he’s in a dark room and he was using, and they charged my insurance company,” said LaRocca.
She digs up an old bill showing $1,200 a pop for urine tests — tests that Shane was faking at a facility in Deerfield Beach, Florida.
“I remember right before I left, I relapsed, and I told them,” said Shane. “And they made sure they got one last pee test. Why? So they could charge me.”
In just one two-week billing period, his insurance was charged $4,800 for urine tests alone.
Aside from insurance fraud, fierce competition for clients has led to another unsavory practice: patient brokering.
“So you think you’re calling a treatment center. And then once you’re there, and they get the prototype of what kind of insurance you have, they then sell your name to the treatment center that will pay the most for you,” said Tieman.
In more extreme cases, middlemen are paid a fee to bring in clients off the street.
These practices are garnering headlines while the industry — as a whole — is trying to clean up its image.
Attorneys general from Florida to Oklahoma are going after patient brokers and drug-testing labs.
Some in the industry say it’s high time they learn to police themselves. Tieman and other heads of large treatment centers are looking into creating a new “good business certification,” so consumers know what to expect from a treatment facility.
The down side of that, he said, is that treatment providers that have not played by the rules will smear the industry’s reputation as whole.
“If we can’t police ourselves, the government and insurance companies will police it for us,” said Tieman.
Right now, there’s a lot of compassion for those battling addiction. But if providers focus more on profits than helping patients recover, they risk eroding that compassion and the political will that comes with it, at a time when health care is in flux.
The Republican-authored health care plan that passed through the U.S. House of Representatives last week would roll back coverage for addiction treatment and mental health care — a massive blow to an industry that already fails to reach most people who need it.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.