Still testing positive after day 10? How to decide when to end your COVID isolation

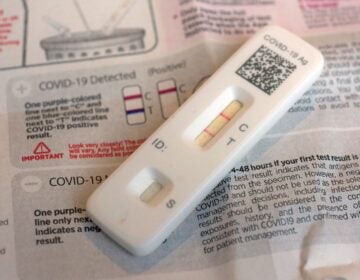
A woman administers a rapid COVID-19 test. (Kimberly Paynter/WHYY)
Many Americans have wrestled with this dilemma at some point during the pandemic, yet it still seems to come up again and again: When can you stop isolating after a COVID-19 infection? The question is especially vexing if you’re feeling better, but still testing positive on a rapid test.
Even with the arrival of new subvariants, the basic ground rules haven’t changed since omicron first came onto the scene: the Centers for Disease Control and Prevention says someone can stop isolating after five days if they’re fever-free for 24 hours and are starting to get better — as long as they keep wearing a mask around others for another five days.
Some researchers have criticized these rules pointing to research that shows some people may remain infectious after day five. And many experts advise waiting until you test negative on an at-home test before venturing out.
But if you feel fine, it can be frustrating to wait, especially if you’re in the subset of those who test positive past 10 days.
James Hay, who studies infectious disease dynamics, remembers earlier this year when his sister continued testing positive for two weeks. Their family had plans to get together over the holiday — a gathering that included an older relative who was vulnerable to COVID.
“To us, that was just not worth the risk,” says Hay, who’s a research fellow at the Harvard T.H. Chan School of Public Health. “Going to the shops with a mask on, that’s a different kind of risk consideration.”
Testing to get out of isolation is tempting because it promises a straightforward answer. Unfortunately — and perhaps unsurprisingly — the science is not entirely settled.
“We don’t have anything that says definitely you are contagious or definitely you’re not,” says Dr. Emily Landon, an infectious disease specialist at UChicago Medicine. “The best thing we have are these rapid antigen tests.”
Unlike PCR tests, which search for genetic material from the virus, rapid antigen tests work by looking for the proteins that are packed inside the virus. A positive test generally correlates with the presence of infectious virus. Scientists can determine that by taking samples from someone who’s been infected and trying to grow the virus in a lab — what’s known as a viral culture.
Generally, most people who get infected are not still testing positive on an antigen test 10 days after symptom onset.
“If you have enough virus in your system to be turning one of these tests positive, that means your body probably hasn’t yet fully cleared the infection,” says Hay.
But there is no perfect study that shows how likely it is that a positive test on a rapid test translates into shedding enough virus that you could actually infect another person, says Dr. Geoffrey Baird, chair of the department of laboratory medicine and pathology at the University of Washington School of Medicine.
“The answer to that is clear as mud,” he says.
Indeed, infectious disease experts tend to differ about how much stock to put in a rapid test result when someone knows they’re infected and deciding whether it’s safe to rejoin the outside world.
After all, Baird points out that these tests were never designed to function as get-out-of-isolation cards. Relying on the result to tell whether you’re truly still infectious is dicey, he says.
“There’s actually a lot more discrepancy than anyone would be happy with,” he says.
A positive antigen test could essentially be picking up leftover viral “garbage,” which can include “dead viruses, mangled viruses … viruses that are 90% packed together but not really going to work,” says Baird. And the amount can vary depending on each person’s immune system, the variants, the stage of the infection, and so on.
This is partly why Baird did not bother to take a rapid test when he had COVID recently and had to decide when it was OK to return to work. After a week, when he was feeling better, he came back to the office, where everyone’s required to wear an N95 mask.
Even if it is an imperfect tool, not everyone is down on using a rapid antigen test.
Landon says it’s extra information that can give you a sense of how to proceed, especially if people are banking on the CDC guidance to determine whether to end isolation. That’s because some people will still be infectious after five days, she says.
In fact, a study co-authored by Landon followed health care workers at the University of Chicago who had been infected but were feeling mostly better and went to get tested after five days. They found that more than half of them still tested positive on antigen tests after six days.
This tracks with other research. For example, one study analyzing data from a testing site in San Francisco during the January omicron surge suggests that many people were still testing positive after five days. And research done by the CDC shows about half of people were still testing positive on the antigen test between five and nine days after symptom onset or diagnosis.
“You’d be erring on the side of caution if you followed the test and said, ‘I’m not going to leave my isolation until after my test is negative,'” she says.
Preliminary data from scientists at Harvard and MIT shows that about 25% of symptomatic people with COVID-19 had virus that could be cultured after eight days after symptom onset or their first test.
But Hay cautions there is considerable variation in the studies because of small sample sizes, differing populations, how the rapid tests are done, the vaccination status of who’s being tested and how healthy they are, among other factors.
“That explains a lot of the variation across studies, but I think it’s still pretty consistent as an overall finding that if you’re antigen positive, then you’re quite likely to be infectious,” he says.
Some research has aligned more closely with the CDC isolation guidance, which assumes most people will no longer be infectious after five days. A preprint study of close to 100 vaccinated college students at Boston University suggests that a majority were no longer infectious after five days.
“Only about 17% of those who we looked at still had what looks like viable COVID out past five days,” says Dr. Karen Jacobson, an infectious disease specialist at the Boston University School of Medicine and one of the study’s authors. A very small number did have virus that could be cultured eight days after symptom onset.
Her study found that a negative rapid antigen test on day five is a “perfect” indicator of whether the virus could be cultured in a lab. In other words, anyone who had a negative test on day five or later after their initial diagnosis had no more detectable virus.
“The flip side was that if you had a positive rapid [test], about half of the people still had culturable virus and half did not,” says Jacobsen. “The way that we’ve started to frame it, and I think many others have, is that if you’re positive, you particularly need to take this very seriously.”
At the end the day, if you’re still testing positive but you feel fine and are symptom-free, the decision to go out in the world comes down to context. If you’re going to spend time with people who are high-risk, think twice, says Landon.
“If you are thinking about going to the nursing home to visit your grandmother, this is not the time to do it,” she says.
But if there’s something essential you need to do, don’t feel trapped in your house. Go do it but keep your mask on, she adds.
9(MDAzMzI1ODY3MDEyMzkzOTE3NjIxNDg3MQ001))


![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)