Philly is ‘floating on opioids’: Civic leaders address drug crisis, share solutions
Philadelphia is wrestling with one of the nation’s highest overdose death rates amid a drug crisis that does not appear to be letting up.

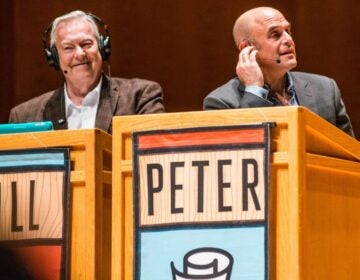
A panel talk on Philadelphia's opioid crisis featured (from left) Maiken Scott, moderator and host of WHYY's The Pulse; Michael McMahon, district attorney of Richmond County (Staten Island), New York; Cynthia Reilly, director of Pew’s substance use prevention and treatment initiative; Evan Behrle, special adviser for opioid policy at Baltimore City's Health Department; Thomas Farley, Philadelphia's health commissioner. (Elana Gordon/WHYY)
Shortly after Michael McMahon won Staten Island’s district attorney’s race in 2015, a young man collapsed on the street where he lived in the middle of the night.
The 22-year-old, whom McMahon had watched grow up, died of a heroin overdose in front of his parents’ house. And so when McMahon started his new job as district attorney, one of the first things he did was ask for the file on that young man’s death.
“I was surprised to learn there was no investigation. It was closed because it was considered an accidental death, and nothing was being done,” McMahon said. “So I sat down with the police department and said, ‘Why don’t we follow up with an overdose and investigate it as if it’s a crime scene?’ ”
From there McMahon, started an intensive overdose response initiative. It has involved investigating and responding to every single overdose, fatal or not, and better coordinating with law enforcement and public health officials. Since then, overdose deaths have finally started to decline on the island.
McMahon recounted this story and the approach he took as part of a panel organized by Pew Charitable Trusts in Philadelphia Friday morning. The goal was to share lessons across cities, as Philadelphia wrestles with one of the nation’s highest overdose death rates amid a drug crisis that does not appear to be letting up.
It’s a stark contrast to a Philadelphia that at the same time appears to be on the way up. Pew’s 2018 State of the City report, released last week, identified promising trends for Philadelphia: a growing economy, an increasing population, flourishing construction. And yet, about one quarter of city residents live in poverty (even more if you consider the higher cost of living in our region compared to the federal poverty line). Drugs are destroying communities and families, with overdose deaths nearly doubling in the last two years.
“The social indicators are unsettling at best,” said Larry Eichel, director of Pew’s Philadelphia Research Initiative, which promoted the opioid event.
What’s to be done?
In 2015, as Baltimore’s overdose deaths climbed, the health commissioner there stepped up overdose prevention efforts, issuing a standing order that allowed anyone to obtain the overdose reversing medication, naloxone, from a pharmacy without a prescription. (Pennsylvania has since followed suit.)
Evan Behrle, special adviser for opioid policy with Baltimore’s health department and a panel participant, said it didn’t stop there. Health workers spread the message “far and wide,” visiting every single pharmacy and distributing the medication to residents deemed most likely to see an overdose.
Teams have also become really aggressive, he said, in responding to overdose data in real time.
“If there’s ever a spike — an unusual number of overdoses — in one really small area, we’ll send an alert, and that’s where we send our outreach teams with naloxone, to do linkage to care,” Behrle said.
Baltimore is also launching mobile treatment vans, to break down “bureaucratic barriers” that often stand in the way of caring for people.
And while the death rate is still high, Behrle said residents who had received naloxone training reported saving 1,800 lives since 2015. Add in police officers and EMS, “it’s well over 10,000 [saves],” Behrle said.
Philadelphia’s health commissioner, Thomas Farley, said he’d get naloxone “into everyone’s pocket” if he could. At about $40 per two-pack, cost is a problem. Meanwhile, he sees the estimated 1,200 overdose deaths that Philadelphia experienced last year as only the “tip of the iceberg.”
Some 70,000 Philadelphians are injecting drugs, Farley estimated, while one in seven residents is regularly taking pain pills.
“This is an entire city that’s floating on opioids,” he said. “And we’re only seeing these different manifestations about the worst aspects of it.”
The city launched an opioid task force last year, prompting new treatment and prevention initiatives in jails and communities. It’s too soon, Farley said, to evaluate those efforts. Meanwhile, the city is grappling with another challenge — how to connect people who want treatment with necessary services right away.
“We still have a strange mismatch where we have a lot of people who say they want treatment, and we actually have a lot of empty slots,” Farley said.
He and other panelists said factors include stigma surrounding the notion of using medication-assisted therapy as a form of treatment, despite strong evidence that it’s more effective than counseling alone. Plus there are “a variety of administrative hurdles.”
If someone is injecting multiple times a day, Farley said, but it takes a day or more to process the paperwork necessary to enter treatment, “that’s too long.”
Farley stressed the need to establish policies so doctors prescribe less opioids, to better connect those who come into contact with the criminal justice system or the emergency room into treatment, and to support the opening of “comprehensive user engagement sites,” or facilities where people could bring their illicit drugs and use them under the supervision of a health worker.
“There is no one solution to this problem,” Farley said. “This is too big a crisis to say we will have one solution. We need to have many different pieces to this. And, let’s be honest, it’s going to take us years to work our way out of this even if we do it all right, right now, given the magnitude.”
Some reasons for hope
Despite the grim numbers and scope of the problem, Felix Torres-Colon said attending the discussion made him surprisingly optimistic.
“It actually gave me a lot of hope that there are these approaches and there are things we think can work,” said Torres-Colon, executive director of New Kensington Community Development Corporation.
He wasn’t on board with everything discussed. While the idea of a safe injection site “sounds good in theory,” he doesn’t want his community to be the testing ground.
“Most historically poor communities have been lied to and mistreated by government, so having a commissioner say, ‘This is a great thing cause this study shows it,’ that’s just not working,” said Torres-Colon.
He was excited to learn about other efforts that were under way, including police diversion programs, peer recovery specialists, and medication-assisted treatment which “just sounds like that beats the heck out of detox.”
“I think we just need more people helping the people get into these programs,” he said. “We need to ratchet that up.”
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.