‘On the frontline of injustice’: Community health workers could improve how long and well you live
Leveraging their shared life experience and local roots, community health workers aim to move the needle on long-standing health disparities.
Listen 4:30
West Philadelphia resident Phyllis Carter (left) takes a walk with her community health worker through the neighborhood. (Courtesy of the Penn Center for Community Health Workers)
About a decade ago, Shreya Kangovi and colleagues at the University of Pennsylvania interviewed 1,500 people in Philadelphia on porches, at hospital bedsides, and in shelters — people who were living in high-poverty communities. All the people interviewed were asked one question: What makes it hard for you to stay healthy?
“Patients told us, for example … that health care providers were constantly setting them up to fail because we give people goals that are not realistic,” said Kangovi, an associate professor of medicine at Penn and a leading national expert on the use of community health workers to improve population health.
“We say, ‘Mr. Jones, you need to take your Lasix,” Kangovi said. “Well, [Mr. Jones] needs to keep his job as a bus driver, and he can’t stop to pee every 30 minutes.”
Kangovi and her team used those interviews to develop IMPaCT, a standardized, scalable program that leverages community health workers — trusted lay people from local communities — to improve health. IMPaCT has been delivered to over 10,000 high-risk patients in the Philadelphia region.
And in the last three years, it has become the most widely disseminated community health worker program in the United States, having been replicated by organizations across 18 different states, including the Veterans Health Administration, state Medicaid programs, and integrated health care organizations.
Kangovi said she thinks of community health workers as a bridge between communities and health systems and other systems of care. Unlike other kinds of health care professionals who are strictly defined by licensure and degrees, community health workers share life experience with the people they serve and often have leadership roles within the community, so they can leverage trust in unique ways.

Typically, community health workers are paired with people in high-poverty neighborhoods who are battling a confluence of health and social inequities, from housing insecurity to high blood pressure.
“We are not actually in the midst of a novel pandemic of coronavirus,” Kangovi said. “But rather what we’re seeing is actually just a manifestation of a pandemic that’s been going on for a much longer time, and that is the pandemic of injustice.”
Despite overall improvements in population health, Kangovi said, health disparities like cardiovascular disease have persisted over time, particularly in marginalized communities of color.
There is about a 20-year gap in life expectancy between the richest Americans and the poorest Americans.
But the primary focus of physicians has been to address risk factors for disease such as smoking or diabetes. And the same has been true of the COVID-19 response in Black, Asian, and Latino American communities, where the death rate is disproportionately higher than that of white Americans.
“What we are calling risk factors are just, in fact, intervening mechanisms,” Kangovi said. “And actually the cause of disease is the underlying socioeconomic conditions.”
Local and federal policies such as immigration and labor laws, neighborhood and domestic exposure to violence, air, and water pollution — these all set the stage for certain groups to have a disproportionate burden of disease.
Kangovi said unlike doctors who focus on treating health outcomes such as diabetes or hypertension on the downstream of injustice, community health workers can intervene at all stages because they share life experience of discrimination and disadvantage with those they serve.
‘Let me find out how I can help myself and others’
At 13, Nahar Alam was forced into an arranged marriage in her birth country of Bangladesh. Alam married a local police officer, and he quickly became physically abusive. Looking for a way out, she fled to the United States in 1993 and found work as a caretaker.
“I came to this country to survive,” recalled Alam. “ But then I worked as a babysitter, and I found so much abuse there which is not reported.”
Settling in Brooklyn, New York, where she had no family to depend on and little English proficiency, she would soon encounter another form of abuse in the homes of her employers. Exhausted and overworked from 12-hour-plus shifts, Alam said she would make as little as $75 a week. And it was common to be denied time off. She even recalls her employers socially isolating her and workers like her by denying them access to the phone.
“And then I thought, let me find out how I can help myself and others,” Alam said.
Stressed by those working conditions, three years later she became a volunteer for Sakhi for South Asian Women, a nonprofit domestic-violence prevention organization. There, she connected with other South Asian immigrant women working as caretakers, cooks, and cleaners in domestic settings who were also experiencing a spectrum of workplace abuses.
“There was nobody to listen to us,” Alam said. “We started the program just to talk to each other, listen to each other, and [do] outreach for each other.”
The women found power in their shared experiences, and together they worked to promote fair working conditions and minimum wage and labor standards, and organized demonstrations outside the homes of exploitative employers. Then in 1998, Alam founded her own organization,
Andolan — one of the first domestic workers’ groups to emerge in New York. Composed of a handful of South Asian domestic workers, Alam and her team helped women through lawsuits against abusive employers and linked them to a range of city services. In 2010, in collaboration with a local labor network called Domestic Workers United, they fought for better working protections and ushered in the first Domestic Workers Bill of Rights.
Alam’s self-advocacy turned into powerful community advocacy. Now, she’s the program associate at the Diabetes Research, Education and Action for Minorities Initiative (DREAM), a community health worker intervention that addresses the burden of cardiovascular disease in New York City’s Bangladeshi community.
“If you hear ‘organizer,’ ‘housekeeper,’ ‘babysitter,’ or ‘community advocate,’ that’s the same [thing] as a community health worker,” Alam said. The same way I advocated for people [then] is the same way I’m doing it now in the health care system.”
‘The advice isn’t tailored to the reality of their lives’
It all starts with outreach. Alam said her initiative recruits high-risk patients from hospitals, doctor referrals, and by word of mouth. Then she’ll contact patients by phone and ask if they want to take part in the program. If they do, she meets with them one-on-one and asks them to set their own short-term health goals.
“I’ll ask them, ‘What do you want to do for losing weight?’” Alam said. “And then they will say, ‘I want to control my food’ or ‘I want to exercise.’ So they set up the time to do that, and then after two, three weeks, we check if it’s working.”
Philadelphia-based Tawandaa Austin is with the Penn Center for Community Health Workers. She said you can’t set health goals for other people.
“You have to allow them to do it, or you’ll have these expectations that aren’t real and that could possibly turn the patient completely off,” Austin said. “So [community health workers] roll with the patient and learn how to be supportive.”

When she’s working with a patient who wants to lose weight, Austin said, there may be other barriers in their way. Perhaps they don’t have the right sneakers, or transportation to the gym is a major hassle. So she meets them where they are and helps them get what they need to succeed.
Alam added that it’s common for doctors and clinicians to tell patients suffering from diabetes and other health problems to eat healthier, without clear or specific suggestions for what healthy eating looks like. She works collectively with patients to teach them about serving sizes and healthy ingredients to incorporate into their food.
Language barriers also are a particular issue for the many immigrant patients who struggle to understand the medical jargon clinicians use to communicate health risks.
For instance, A1C is a blood test for type 2 diabetes and prediabetes. It measures your average blood glucose, or blood sugar, level over the past three months. Doctors may use the A1C alone or in combination with other diabetes tests to make a diagnosis. Alam said doctors often tell her patients to lower their A1C levels.
“I think 100% of [my clients] don’t know what A1C means, so we teach them,” Alam said.

Nadia Islam is a professor at NYU’s School of Medicine who oversees Alam’s community health worker program. According to her, instead of thinking about ways in which the health care system is hard to access for a large segment of the population, it’s more common to hear from doctors that patients just don’t want to listen and take advice.
But community health workers are able to bring their understanding of the patients’ lived experiences to the work they do. Many of Alam’s clients work very sedentary jobs.
“If you think about taxi drivers who work 12-hour shifts,” Islam said, “they need to think about where they can park their cars to be able to take breaks. So they’re often eating on the job with very little opportunities for physical activity.”
“So it’s not so much that patients aren’t listening, but that the advice that they’re given isn’t tailored to the reality of their lives.”
Community health workers lead nutritious-cooking tutorials and disease-specific education classes with their clients, giving them the tools and opportunities to practice lifestyle changes on their own terms. They accompany them to doctors’ appointments, where they can break down medical terms, and check in with patients in real-time to ask them if they understand what the doctor communicated.

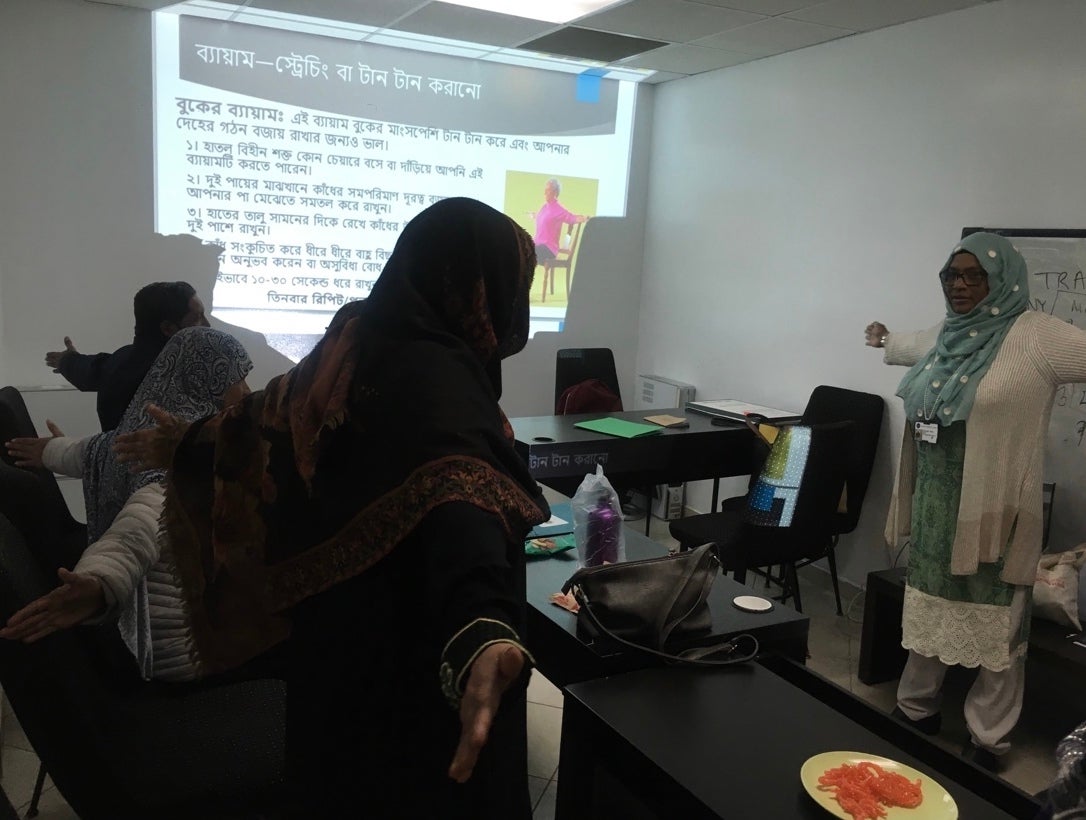
In addition, community health workers like Alam and Austin implement culturally relevant physical fitness opportunities, like yoga classes or gender-segregated classes. And they have also done a lot of work with local businesses to promote positive health contexts.
“Being almost predominantly an immigrant population, the Bangladeshi community has a strong network of sort of immigrant-owned small businesses, including ethnic grocery stores and restaurants,” Islam said. “And so a lot of our community health workers do things like working with grocery stores to do product placements of healthy items, like culturally appropriate healthy items like brown rice or like fruit and vegetable displays.”
But Austin said her clients also see her as a source of reprieve and community. It’s not all about meeting immediate health needs, but rather about creating a culture with clients that makes them feel cared for. During the COVID-19 pandemic, that’s been all the more important, as many of the people she works with are battling social isolation and have lost many loved ones to the virus.
“I have some patients who just like to talk to me, so they might call me, and it can be anything from if we want to FaceTime or do like chair yoga together,” Austin said. “Just kind of still trying to be normal [during] this un-normalness that we have going on.”
Health inequity as a psychological distortion
Kangovi uses her community health worker research to push clinicians to understand health inequity as a kind of psychological distortion of privileged people. She said doctors want to help, but they often don’t share the same life experience as their patients, which leads to things like savior thinking and group narcissism.
Kangovi noted that there’s a neuroscience experiment that tracks what people are looking at when they walk through a neighborhood. She said the study found that wealthier people do not even see people they perceive to be of a lower socioeconomic status than themselves.
“And those psychological distortions like racism or greed make their way into public policy, which affects the distribution of wealth and power across society,” Kangovi said. “This affects people’s living conditions, which of course influences their behaviors, and that is a major determinant of health.”
The community health worker model acknowledges that health care infrastructures are also a part of this system of privilege, and that doctors sometimes even perpetuate and benefit from these systems. Kangovi said doctors and clinicians have a limited biomedical view of the kinds of skills it takes to address health inequity. There’s an overemphasis on clinical training and educational qualifications, but community health workers have a unique skill set, bolstered by shared lived experience and deep community roots, and are defined by what Kangovi described as “compulsive levels of altruism.”

Alam recalled a former Bangladeshi immigrant client who kept missing her checkup appointments at her hospital. The client was diabetic and in need of urgent care, but the doctor had no idea why she was not showing up. After many attempts to reach her by phone, Alam visited her home. She quickly discovered that her client didn’t know how to use public transportation on her own or travel without the aid of her husband or son, who were working for most of the day.
“She didn’t know how to read [in English], so I showed her the building color and the shopping center and the sign there in the subway station, so she could recognize it when she came off [her subway stop for the hospital],” Alam said.
Alam said she remembers trying to navigate New York herself during her early days in this country and the challenges of trying to access city services and health care with little to no English. Weeks after showing her client how to use public transportation, she had trouble reaching her by phone again. Then out of the blue, the client called her back to say she’d been busy for the past week traveling throughout the city by bus, doing grocery shopping, and visiting family in other parts of New York.
“Her lifestyle was changing,” Alam said. “She learned how to go outside and meet the doctor, she was so excited.”
‘We do experience what the patient is experiencing’
Community health workers like Alam break down barriers for all kinds of patients, barriers to care doctors don’t have time to address from their practices. And this special workforce actually leads anti-racism and social justice interventions for clinicians and policymakers who lack the lived experience of discrimination and disadvantage.
At Philadelphia’s Penn Center for Community Health Workers, CHWs lead a rotation for clinicians and health system executives, who shadow them for several days in the communities they serve.
Community health worker Tawandaa Austin said she has many patients who live in areas of Philadelphia where public transportation is close to nonexistent and they struggle with physical mobility.
“So I would take those doctors and nurse practitioners to those places, and we do walk, we do experience what the patient is experiencing,” Austin said. “Or if [the patient is] in a high-rise project complex, we do have to walk up or down those steps [to] let [doctors] know what it’s really like. So we kind of bring everything to the light.”
Kangovi said clinicians tend to hire one another and hold onto power, which just reproduces the same clinical models that continue to contribute to the widening of health disparity. But when doctors transfer that power to people like Austin who are more skilled at addressing the root causes of poor health, there’s a real impact on health outcomes for many high-risk patients.
Whether you’re dealing with a patient who suffers from addiction or heart disease, Kangovi said the approach of getting to know who patients are and what they want and need actually seems to move the needle on long-standing health disparities.

Results from three randomized trials Kangovi led with her team at Penn showed that community health worker interventions reduced the frequency of hospitalizations and length of stay in hospitals for high-risk people like Alam’s diabetic client.
“Typically what you see is that there’s a very intensive social behavioral intervention that moves the needle,” Kangovi said. “But as soon as it ends, there’s a voltage drop, and things go back to the way they were.”
So the effect of a community health worker intervention, at least on hospitalizations, actually persists long after the community health worker says goodbye.
Kangovi said researchers are not quite sure why yet, but Alam has a theory. She said she wakes up to calls from clients and ends the day with these calls as well. Typically, she has various one-on-one sessions with a client over a six-month period, and then she moves on to new cases. When asked about what happens to those people after the intervention period ends, she had this to say:
“You use the word ‘end’ but… there is nothing like that because [clients continue] calling me,” Alam said. “Maybe I can say my program is finished, but nothing for them is finished because this is where I’m from, I’m from the community.”
Strong attachments, personal investments, and deep trust emerge between community health workers like Alam and Austin and their clients. These are not relationships they can just walk away from, and they don’t. They continue to be resources and listening ears for those they served for months and years to come.
“So we have a slogan: Do it now,” Austin said. “People want to have their needs met right then. So the thing I want to do is make people feel like they’re heard. How are you feeling? I hear you. Let’s do it together, let’s do it now.”
—
Support for WHYY’s coverage on health equity issues comes from the Commonwealth Fund.
 WHYY is one of over 20 news organizations producing Broke in Philly, a collaborative reporting project on solutions to poverty and the city’s push towards economic justice. Follow us at @BrokeInPhilly.
WHYY is one of over 20 news organizations producing Broke in Philly, a collaborative reporting project on solutions to poverty and the city’s push towards economic justice. Follow us at @BrokeInPhilly.

Get daily updates from WHYY News!
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.






