Penn doctor uses his near-death experiences to research why COVID-19 patients crash
Facing the cytokine storm — David Fajgenbaum brings his first-hand experience with cytokine storms to bear on this new coronavirus.
Listen 09:10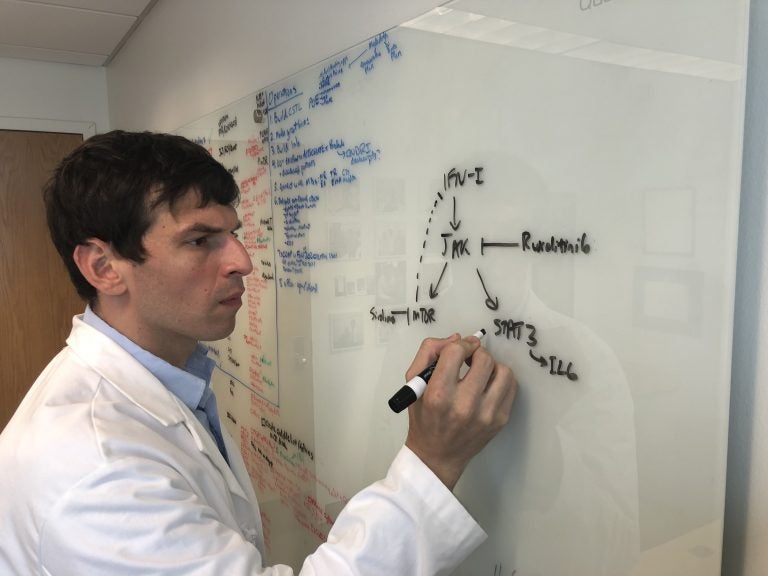
David Fajgenbaum leads a research lab at the University of Pennsylvania dedicated to studying Castleman disease, a rare illness that nearly killed him five times. He has recently shifted his focus to look at ways of treating COVID-19. (Courtesy of David Fajgenbaum)
This story is from The Pulse, a weekly health and science podcast.
Subscribe on Apple Podcasts, Stitcher or wherever you get your podcasts.
In a best-case scenario, symptoms of coronavirus might be nothing more than some fatigue, a slight fever, and a dry cough that settles at the back of the throat. But at its worst, COVID-19 can send patients into a sudden crash — an extremely painful experience — known as a cytokine storm.
It’s a type of immune system hyperactivation in which the body is bombarded with signals that push the immune system into overdrive. The cytokine storm itself can cause more damage to the body than the viral invader the storm is trying to fight.
“This happens in a setting where your immune system is trying to fight off the virus,” said David Fajgenbaum, a physician and researcher at the University of Pennsylvania who specializes in Castleman disease research and cytokine storm disorders.
He says your immune system “gets so ramped up in trying to fight the virus that actually it basically just gets out of control and … rather than just targeting the virus, now you have the immune system targeting all of your healthy vital organs.”
Fajgenbaum has personal experience with cytokine storms: He’s lived through several of them. Since 2012, he’s battled Castleman disease, a rare illness that has features both of cancer and an autoimmune disease. Fajgenbaum’s diagnosis has guided his work and research. He’s written about his journey in his book, “Chasing My Cure: A Doctor’s Race to Turn Hope Into Action.”
“I’ve lived like this for the last 10 years, basically, with the fear of the unknown that so many of us in society and across the world are now living with.”
As concerns about the coronavirus intensified in the U.S., Fajgenbaum remembers thinking to himself: “I hope a lab out there begins to apply some of the things that we’ve learned about Castleman disease and cytokine storms to COVID-19.” He hoped that those researching COVID-19 would look into treating this immune hyperactivation and not just focus on the virus itself.
“And then I found myself saying, ‘Wait a minute, you know, if I’m going to hope that someone out there does it, we’ve got a lab that’s focused on this, and we’ve got people who were committed to making a difference in other patients’ lives. And so why don’t we just do it?’”
Fajgenbaum sprang into action and assembled a 30-member team of scientists, many of whom are members of the Castleman Disease Collaborative Network and had been working on similar research before the pandemic. Together, they’ve attempted to systematically capture data on treatments for COVID-19, to see what’s been working and what hasn’t, to find out which existing drugs could be most effectively repurposed to battle this disease.

“I think a fitting analogy for what we have tried to do would be when you think about a wartime scenario,” said Fajgenbaum. “Our front lines have all gone to battle against COVID-19. And they’ve tried a number of different drugs against it. Some things have worked, some things have not worked. Now that we have basically the second wave of physicians fighting against the second wave of patients right now, we need to arm those physicians with information and data on what actually worked during the first wave.”
Together, they’ve scoured over 2,500 published papers and have extracted data on over 100 drugs used in more than 9,000 patients reported to have COVID-19.
“And now we have, what I believe as of right now, is the world’s only central database that lists all the drugs that have ever been tried against COVID-19.”
Although this work will set Fajgenbaum back on his initial Castleman disease research, he feels compelled to put his energy into the fight against COVID-19.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.




![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)