Navigating the realities of relapse amid recovery
When it comes to recovery, relapse is common. But it doesn't have to be inevitable.
Listen 9:26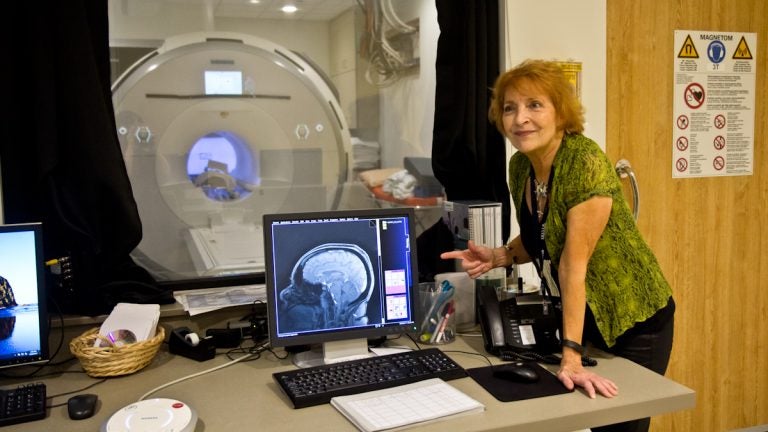
Dr. Anna Rose Childress is a leading neuroscientist at the University of Pennsylvania's center for addiction studies. She has spent decades scanning and observing the brains of people who have experienced addiction. (Kimberly Paynter/WHYY)
For decades, prevailing wisdom held that to overcome addiction, the most important thing to do was to flush or “clean” the drugs out of one’s system, to get a fresh start. But more and more, research into the brain, in particular, has largely found this notion to be a myth. After all, long after those chemicals are gone, the underlying addiction and the cravings are still there.
It’s a reality that’s underscored by the high rates of relapse during many people’s recovery process. And it has scientists and others looking even more deeply into the moment of relapse, to better understand the challenges and opportunities that can better set one up for success. That’s even more important nowadays, given the higher stakes, with a rise in overdose deaths and an increasingly potent illicit drug supply, if one were to relapse.
Back in the lion’s den
The story of Nate Robinson reads like a history text for drugs in America. In the 60s and 70s, he says it was “the hippie time,” with lots of alcohol and marijuana use. It was also the early days of meth. In the 80s, it was cocaine and then crack.
“You know, it’s like a euphoric feeling. Once that wears off, you want another hit,” Robinson recalled. “You spend your whole paycheck that night.”
Then, in the 90s, came heroin.
“By ’97 I looked like a 60-year-old man, and was in my late 30s. I lost all the weight,” Robinson said. “I’ve been a slim dude all my life anyway, but now I’m done. I mean I’m burnt.”
It was at that point that Robinson said he went into treatment for the first time. It changed his life, from the time of detox, through rehab, and into a recovery house, he was boasting that he was “14 months clean.”
He landed a job in guest services at a hotel. He was feeling incredible.
“Oh my god! I haven’t felt this good since my early 20s,” Robinson said.
But then, “Boom boom boom!”
He relapsed.
“This particular day, I rode down the wrong neighborhood, putting myself right down the lion’s den, as you call it,” Robinson said.
He saw people getting high, and it was all downhill from there.
Robinson has been in and out of treatment since, but his story is not an uncommon one. When it comes to addiction and recovery, relapse is often a reality. One Harvard researcher, Dr. John Kelly, found in reviewing lots of retrospective and prospective studies on addiction, that people may still be really susceptible to relapse for many years after getting into recovery.
“So, for example, we know that to get one full year of full sustained remission, it can take several years, it can take four or five treatments, and roughly eight years on average before people achieve that first year,” Kelly said.
So why is it so darn hard to quit, to clear out an addiction?
Finding clues in the brain
It’s a simple question with a very complicated, nuanced answer that has a lot of moving parts.
According to the American Society of Addiction Medicine, the risk of relapse after periods of abstinence is a “fundamental feature of addiction.” Triggers include “exposure to rewarding substances and behaviors, by exposure to environmental cues to use, and by exposure to emotional stressors that trigger heightened activity in brain stress circuits.”
The society doesn’t go so far as to pin down any specific average number of times or time frame for relapse risks, instead noting that relapse is not inevitable, that clinical interventions can be effective in altering that course, and that the ways that people respond to drug exposure and addictive behaviors “are different at later stages of addiction than in earlier stages.”
Relapse also varies by person, by experience, by triggers, trauma, the severity of the addiction to begin with, and the stressors in a person’s life, both the bad and the good.
“So people, when they get into recovery can have good things happen, like getting a new job, moving to a new city, getting a new relationship, all those factors actually can be risk factors for relapse, ” Kelly said. “You might be more vulnerable when you move to a new area with a high-stress job, When you can’t get connected to a recovery support system, that can make people vulnerable.”
This cycle of relapse, and what makes some more prone to it than others, is also something that scientists like Dr. Anna Rose Childress have been slowly trying to crack, by cracking a lid on the brain itself.
Childress, a leading neuroscientist at the University of Pennsylvania’s center for addiction studies, has spent decades scanning and observing the brains of people who have experienced addiction, trying to zero in on that moment of relapse, to figure out how to prevent it. She scrutinizes what happens, for example, as activity in the amygdala and mid brain picks up, where dopamine has its origin.
There’s an old saying in the recovery community that the people, the places and things need to change. Childress says it goes beyond that.
“One of the things that was intriguing to me is that people would sometimes come to me with accounts of, ‘You know, I don’t know what triggered me. I really don’t know. I was OK one minute. I was fine. I was sitting there minding my own business, having breakfast. And then the next thing I knew, I felt incredibly pulled. I was on a mission. I was out the door. I don’t know what happened to me,'” Childress recalls of her patients’ accounts.
At a closer look, Childress says the brain contains a really powerful reward system, a circuitry, that for thousands of years has been essential to the survival of humans. It’s the one that lights up and goes nuts, increasing activity and releasing chemicals, during opportunities for sex and food.
“This is the absolute priority for our brain, is to make sure that we respond to those rewards so that we stay alive and pass on our genes,” said Childress.
That reward system is stronger in some people than in others. This carries a sort of dark irony because this would have been a huge advantage during any other time in our evolutionary past.
“The very brain that essentially would make us the fittest of the fit, right, that we would be the first to find the food, having sex, keeping our genes going, that brain is now the brain that is at greatest disadvantage in these last eye blinks of history,” she said.
The rules of survival have changed, but drugs can put this reward system into overdrive and teach it to continue seeking out such powerful highs.
But it’s not just the brain’s reward system. It’s the brain’s brakes, too. In the same way that, at some point, a person has to stop eating all the cake (and, meanwhile, some people are better at refusing an additional slice), drugs weaken those brakes.
“Some drugs of abuse – stimulants like cocaine and amphetamine – with chronic exposure to these, regardless of where your break started, actually erode your breaking power,” said Childress. “You’re rubbing them out.”
To get a sense of how powerful brain chemistry is, Childress has run a series of MRI experiments where she flashed for just 33 milliseconds a photo of drugs in front someone with addiction. The flash, among other more sustained benign photos of things like fire hydrants and buildings, happened so fast that one wouldn’t even notice it. But she saw even that flash of an image still triggered the reward system, lighting up that part of the brain in participants.
“And so we’re good storytellers about why we did as though we decided it, but some of it actually is occurring outside our awareness,” Childress said. “So that’s another piece of the picture, is that not all of our decision making is nearly as conscious as we would like to think it is. But whatever amount of it we had that was consciousness and deliberate and essentially good decision making, often gets eroded by this disorder in a very biological way.”
That a person is not consciously steering the brain’s engine may be an overbearing notion to grasp.
“It’s essentially taking away some of what we like to think of as our essence,” said Childress. “And so part of recovery is trying to get back your decision making ability. Because that really is very close to who you are.”
This is why for many in the addiction community, including Childress, the use and advancement of medication assisted therapy, like methadone, buprenorphine and naltrexone – which in different ways blocks or fills those reward systems for certain drugs – is so critical.
What’s less known, though, is how the addicted brain and those systems change and evolve over time in recovery. That work is much harder to do and is just beginning. A massive federal study, for example, will soon follow the brains of teens over time with the hope of better understanding how some brains respond better in the face of addiction compared to others.
From ‘moral failing’ to chronic disease
So, does all this mean relapse is inevitable?
“People conclude that it’s a moral failing, that recovery is not possible,” said Dr. Rose Julius.
But, that’s not true, not even close, she says.

“We don’t come to any of those conclusions with any other chronic condition,” said Julius, who oversees addiction services for Philadelphia’s large medicaid population as deputy chief medical officer at Community Behavioral Health. “It does not mean that you have to live with this sort of negative albatross around you forever.”
Julius is well aware of the realities of the current addiction landscape: according to her agency’s medicaid claims, more than half of people who go through detox have relapsed.
What she says that means is that a shift needs to happen, one that matches the base of evidence out there for treatment approaches: that addiction, like diabetes or asthma, can be properly managed if it’s treated as a chronic condition, one that requires personalized, ongoing supports and treatment, long term. Detox, she stresses, and the long-held inclination to just clear a chemical out of one’s body, can’t be viewed as the treatment itself.
“I treat lots of people with addiction, and the most common thing I hear when people relapse and we talk through ‘well, what do you think happened?’ – in addition to being exposed to certain things that are triggering for that individual, you often hear most commonly that someone stopped doing the things that was keeping them in recovery,” Julius said. “So they would stop attending support groups, stop attending treatment. You know, basically forgetting about the things that they were doing proactively that was helping to support them.”
Julius says part of the path toward successful recovery is building long term coping skills, especially in the face of a relapse risk, but also amplifying the message that recovery is possible. She sees that with patients all the time.
And, it’s why just a few weeks ago, thousands took to the streets in Philadelphia in support of each other and their successes, large and small, during a massive recovery celebration.

“I need to be down here, I need to be a part of this,” said Steven Scott Jr., with a booming smile. “I need to see I can actually do this, and if others can do it, why can’t I?”
Bob and Nancy Lamb came to support their son, who is in year five of recovery.
“It’s been such a struggle as a family unit,” Nancy Lamb said. “Sobriety is amazing.”
“You always think that you’re alone when you’re out there, but here a lot of people have the same stuff, I wish I’d known them before,” said Jennifer Burke.
“There’s nothing wrong with starting over and opening up and telling people what you need, that you need help. You can’t do it alone,” said Candy Lee.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.






