“Nobody’s Normal:” reducing mental health stigma
Professor Roy Richard Grinker discusses how mental illness became stigmatized in America and our progress toward a culture more accepting of mental health differences.
Listen 49:00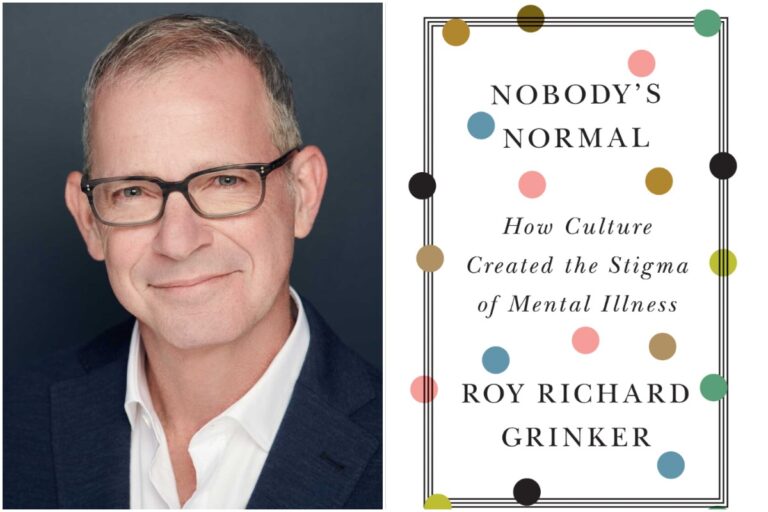
People who suffer from mental illness have too often been marginalized and hidden from sight and society. In his new book, Nobody’s Normal, anthropologist ROY RICHARD GRINKER examines the history of mental health stigma in this country, why “normality and abnormality are fictional lands,” and our progress toward a culture more accepting of neurodiversity. We’ll talk to Grinker about the history of our attitudes to mental illness, his family’s four generation involvement in psychiatry, including working with Sigmund Freud, and his daughter’s experience with autism.

Subscribe for more Radio Times
Interview highlights
On the roots of mental illness stigmatization:
Marty Moss-Coane: It’s interesting to think about the roots, as you write, of the stigma of mental illness, knowing how common it is, whether we’re talking about anxiety or depression.
Roy Grinker: Yeah, it’s really fascinating, the roots of it, the roots of stigma are not just in the sort of history of industrial societies in which we have sought to value highly people who produce a lot and to negatively value those who don’t, to value people who can be independent and negatively value people who are dependent. But it also intersects with racism and sexism and classism and all forms of other discrimination. So if we think about mental illness, stigma in isolation, we don’t see the full picture, which is that African-Americans in this country were often denied any kind of psychological care. Even today, children with autism who are African-American are diagnosed later or misdiagnosed and not given the same kind of accommodations as their white counterparts. Women were thought, and often are still thought, to be more prone to mental illness. And class also has played a huge role throughout the course of the 20th century. So it’s important that we see that mental illness stigma is part of a larger, kind of deep structured, institutionalized process.
On mental illness and prisons:
MMC: Now what we read is that the prisons have become the new mental institutions, and that’s where people go because you cannot, you know, have some kind of long term hospital facility to take care of someone’s enduring mental illnesses.
RG: That’s true. Prisons are the number one provider of mental health care right now. The idea of deinstitutionalization in the early 60s, the Community Mental Health Act, was the last law that President John F. Kennedy signed before he was assassinated. The idea was to bring people into the community, to release them from these deplorable institutions and asylums. But what happened was that the funding wasn’t there and the political enthusiasm wasn’t there. And it ended up basically dumping people onto the street. And so homelessness and all kinds of other conditions, including severe poverty, resulted. I mean, so much so that some people who advocated strongly in the past for deinstitutionalization are having second thoughts.
On mental and physical illness:
RG: We can’t say there are mental illnesses and there are physical illnesses because the two are intertwined. It doesn’t really make sense to separate those out. People who are suffering from all kinds of physical illnesses have mental health consequences. Mental health itself affects our physical being. And so I think that there aren’t enough multidisciplinary teams out there and there are not enough people who are integrating both medical care and psychiatric care to account for what used to be called psychosomatic conditions.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.





