Sore arms, role models, and relief: Philly region health care workers on the COVID-19 vaccine
What’s it like to get the COVID-19 vaccine? Some of the first people to receive it described how it felt to WHYY’s Health Desk Help Desk.
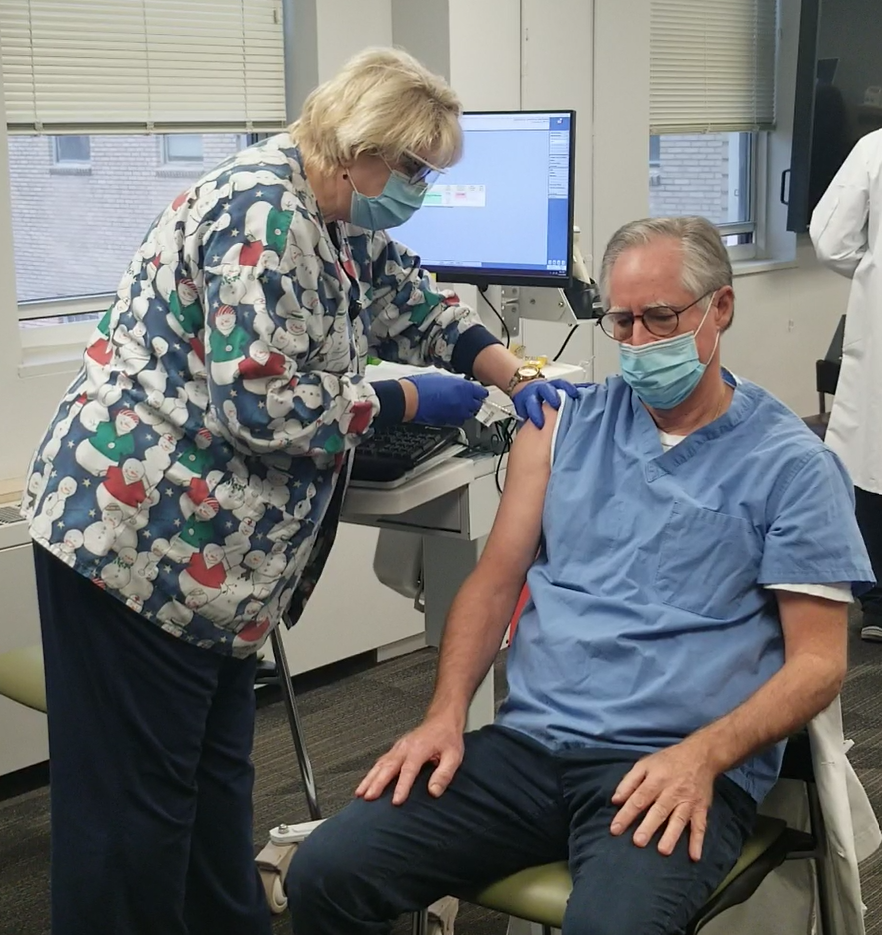
Listen 5:43![Dean Johnson recieving covid vaccine[1] Robert Johnson, dean of Rutgers New Jersey Medical School, receives his first COVID-19 shot.](https://whyy.org/wp-content/uploads/2020/12/Dean-Johnson-recieving-covid-vaccine1-768x431.jpg)
Robert Johnson, dean of Rutgers New Jersey Medical School, receives his first COVID-19 shot. (Erico Rovayo/Rutgers University)
Ask us about COVID-19: What questions do you have about the current surge?
WHYY’s Health Desk Help Desk heard from a lot of listeners with questions about what it’s like to actually get the COVID-19 vaccine. So we reached out to some of the very first people to receive it: health care workers. They told us how they felt afterward, and how it would change their personal and professional approach to the pandemic going forward.
___
Whitney Cabey
ER doctor, assistant professor of emergency medicine, Temple University Hospital
Whitney Cabey got the COVID-19 vaccine two weeks ago. In part, she wanted to set an example.
“I’m a Black woman, I’m a Black mom, so I feel like I’m … just taking in a lot of people’s questions, their concerns, their fears,” Cabey said.
On the way home from getting the vaccine, she was feeling good. She climbed into an Uber and started chatting with her driver.
“She shared with me that her father had gotten extremely sick from coronavirus,” Cabey recalled. She asked the driver if she was planning on getting the vaccine, since she’s transporting people as a frontline worker. The driver told Cabey she was still very nervous — she didn’t want the side effects, and said she doesn’t usually get the flu vaccine.
“I was really kind of struck by that, because she saw the face of COVID, she would never want it for herself, she wants to protect her mom and the rest of her family, but still the fear is there and the fear is very real,” Cabey said. “So it just makes me aware and humble in terms of understanding that we do have this uphill climb.”
Cabey told her driver that she’d just gotten the vaccine, and wasn’t feeling any effects.
The driver remained unconvinced.
“That time, it didn’t work,” she said.
Cabey said this illustrates how important it is for people to hear about the vaccine from their family doctor, block captain, church leader — someone they trust.
Lynda Thomas-Mabine
Chief of gynecology, Chestnut Hill Hospital
One of those people is Lynda Thomas-Mabine. Even before she had decided to get the COVID-19 vaccine, she said, her colleagues, especially people of color, were asking her about it. She said that made her realize she could set an example.
“Many of them were saying, ‘Dr. Thomas, if you get it, I will get it.’ And so what I did was I videotaped me getting my vaccine, I had one of the other nurses taking the picture, and I purposefully went around and said, ‘Hey, I did it today. When your turn comes, I want you to also get your vaccine.’”
She said all her colleagues asked her how she felt afterward. She replied that she felt great, safe, and that her family is going to be OK. Her family has also talked to her about their skepticism of this vaccine.
“I have an 87-year-old mom, who was reluctant to get the vaccine. As an African American, many of us are skeptical about racism in medicine, and discriminatory responses in health care that some of us have experienced and talked about; Everyone talks about the Tuskegee experiment … which was a long time ago. I said, ‘This is a new day.’ And they need to have confidence that health care is going to do what they need to do to keep them safe, especially during this pandemic, and they have me as an advocate.”
After Thomas-Mabine got vaccinated, her family celebrated, and she got text messages and calls.
“They worried about me every day as the only physician in the family … My siblings, my mom, everybody was just thrilled and applauded, they worried about my safety, and now they feel relieved that I am going to be OK, and I’m hopeful that they will get the vaccine as well.”
She said she is feeling much better, as well.
“I woke up … with this clarity, this sense of wellness, that I haven’t felt in a very long time,” Thomas-Mabine said. “I realized that the stress of … knowing that every day I could potentially have been exposed, I could have potentially have gotten COVID, that’s gone now. I feel emotionally a sense of euphoria that I haven’t felt in the nine months that we’ve been going through this.”
Tyler Coty
Nurse, Bayhealth Medical Center
Tyler Coty, too, felt nothing but thrilled. He works in an ICU designated for COVID-19 patients at Bayhealth Medical Center, and when his hospital issued a signup list for the vaccine, he put his name down immediately.
“I was super-thrilled about the fact it was coming out, and all the studies had been done and everything looked good, so it was something I was looking forward to,” said Coty, who works with critically ill COVID patients. “I was excited about the effort that was made to crush this virus, and if it’s something I can do for my patients, I’m all for it.”
On the day he was vaccinated, Coty said, he went down to the designated area and watched as one of his co-workers became the first person to receive the vaccine at the organization.
“I kind of witnessed a historical moment,” he said. “I was very thrilled and looking forward to it, and it was nice to see the excitement with everyone else involved too.”
He said he had a sore arm for about 24 hours, but it was very manageable, and he had no other side effects.
“The benefits outweigh the risks,” Coty said. “Think about all the individuals who have suffered and died from COVID. This is one step we can take as a population to save the vulnerable folks in our society. It was a risk I was willing to take, and it’s a risk the public should consider taking to nip this in the bud.”
Gregory Berry
Lead hospitalist, Nazareth Hospital
Back in March, so many of Gregory Berry’s colleagues got sick that he moved into an Airbnb for a month. His partner is also a physician.
“We both realized that the infection control was breaking down, not only at this hospital, at a lot of hospitals,” Berry said, adding that it was a dire time. “We had no treatments that were proven, we had shortages of PPE, we were floundering.”
“Since then, we’ve recovered, but we haven’t felt we’ve put this behind us … I haven’t moved out, but we do social distance at home.”
Berry said he and his significant other have separate bedrooms, watch TV in the same room but stay 6 or 12 feet apart. He showers immediately after coming home, and his clothes stay in a particular part of the house.
He said they have been doing that since the most recent surge, when his hospital has been at capacity.
“We are seeing more than half of our patients in the hospital now have COVID … we have to hold patients in the emergency room, in the hallways, he said. “We have not run out of ICU beds yet, but we’ve been at 90, 95% consistently. The floors are full, we have empty wards where we could put more patients, but nursing is a problem.”
He added that his colleagues have managed to treat all the patients who come in, and he knows it is worse in states like Texas and California.
“However with the vaccine, there’s an exhilaration, a sense that we can get this under control. The morale now is incredible in the hospital, it’s the first time we are feeling lighter in our step, even with the surge, which is difficult right now, we have hope, and we were all looking for something to sustain us through this surge and the vaccine has done it.”
Astrid Colon Torres
Social worker, Nemours/Alfred I. duPont Hospital for Children
A few weeks ago, Astrid Colon Torres’ mother sat her down and asked if she would take the vaccine if it was offered to her. She provided an answer she thought would reassure her mother about the vaccine’s safety.
“I said, ‘Yes,’ because I wanted some of my older family members with underlying conditions to have some hope and not live in fear,” Colon Torres said.
Fast-forward about three weeks, and Colon Torres showed up to her workplace full of nerves and hope to be among the first to get the shot.
“There was a lot of excitement there, there was no negative cloud in the whole room,” she said. “There were a lot of positive vibes.”
After the vaccine was administered, staff were asked to wait 15 minutes for observation, to make sure there were no immediate side effects before sending them back out to the community.

Colon Torres didn’t have any adverse side effects, but she did experience chills the night she received the vaccine and also had arm pain for more than a day.
She recommends that people talk to their doctors before getting the vaccine, especially if they have underlying conditions. She also suggests that people do their research but be skeptical of what they see floating around on social media, much of which is inaccurate.
Colon Torres said it’s important that she and others in the health care industry make an effort to share with people of color that the vaccine is safe.
“I’m well aware there aren’t a lot of people in the higher positions in health care that look like me, that speak Spanish at home like me, that have similarities to my life experiences, so I think that’s what pushed me to, ‘Well, if I’m just that one Puerto Rican that people see, maybe it will encourage them to do more research, not necessarily get the vaccine, but have a little more trust in medical systems,’” she said.
The day after Colon Torres received the vaccine, she worked with a 17-year-old Black girl who was in the hospital to get tested for COVID-19. The girl asked her and the respiratory therapist if they had received the vaccine.
“I was very happy and proud to tell this patient, ‘I do and I have it inside me right now.’ She didn’t ask follow-up questions, but I could see her kind of gauging, ‘I’m here at a hospital, and I want to see how many professionals here are entrusting this vaccine,’” Colon Torres said. “So representation is important. As health care workers, it’s important for us to illustrate we do have trust in science, and yes, we’re weary and just as nervous as you guys, but we’re going to illustrate we do have trust in science and our hospital.”
Erica Harris
Emergency physician, Einstein Medical Center
Emergency medicine clinicians have a tendency to walk directly into the fire.
“Especially when you’re dealing with critically ill patients in emergency medicine — that’s what we’re trained to do,” said Erica Harris, an emergency doctor at Einstein Medical Center. “You run towards the emergency, you don’t run away from it.”
Because this is second nature for so many people who work in the emergency department, Harris said, they don’t have time to stop and be afraid of whether they’ll get COVID-19 while changing the breathing tube of a person on oxygen support or performing another risky procedure. They simply do it. It’s when they get home that all that built-up stress comes crashing down.
“By the end of your shift, you have this cumulative effect for caring for so many patients that could potentially make you sick that you kind of recognize it at the end,” she said.

Harris, who was one of the first people at Einstein to receive the vaccine, said that she knows the first shot doesn’t mean she’s immune and that even after her booster in a few weeks, she won’t know for sure, since we don’t have data yet on whether people who are unlikely to get sick with COVID-19 can still be carriers and transmit it to others. She’s not planning to change her behavior.
“I think of it like an insurance policy,” Harris said. She still plans to wear a mask and other necessary personal protective equipment at work and outside work, she said.
But she is hoping that the constant psychological stress will be alleviated.
“We all live with this fear of, “Will this be the time that I catch this?’” she said of herself and her fellow health care workers. That’s what she’s hopeful will change.
“In the coming months, they know they will be at less risk and have less of that burden to bring home. It’s a gift.”
Michael Kirchhoff
ER physician, patient safety officer, Cooper University Health Care
Most doctors don’t get excited about vaccines. They get the flu shot every year — it’s part of their regular routine.
This one was different.
“Honestly, I got a little teary at the end there,” said Michael Kirchhoff, who was one of the first 30 people to get vaccinated at Cooper University Health Care. He described a scene that was more like a giddy line of fans waiting in line for a concert than a vaccination.
“You’re seeing that light at the end of the tunnel, and it was very moving … When I got my vaccine, it was clapping and cheering, it felt something other than, it felt more like a graduation than a vaccination, honestly.”
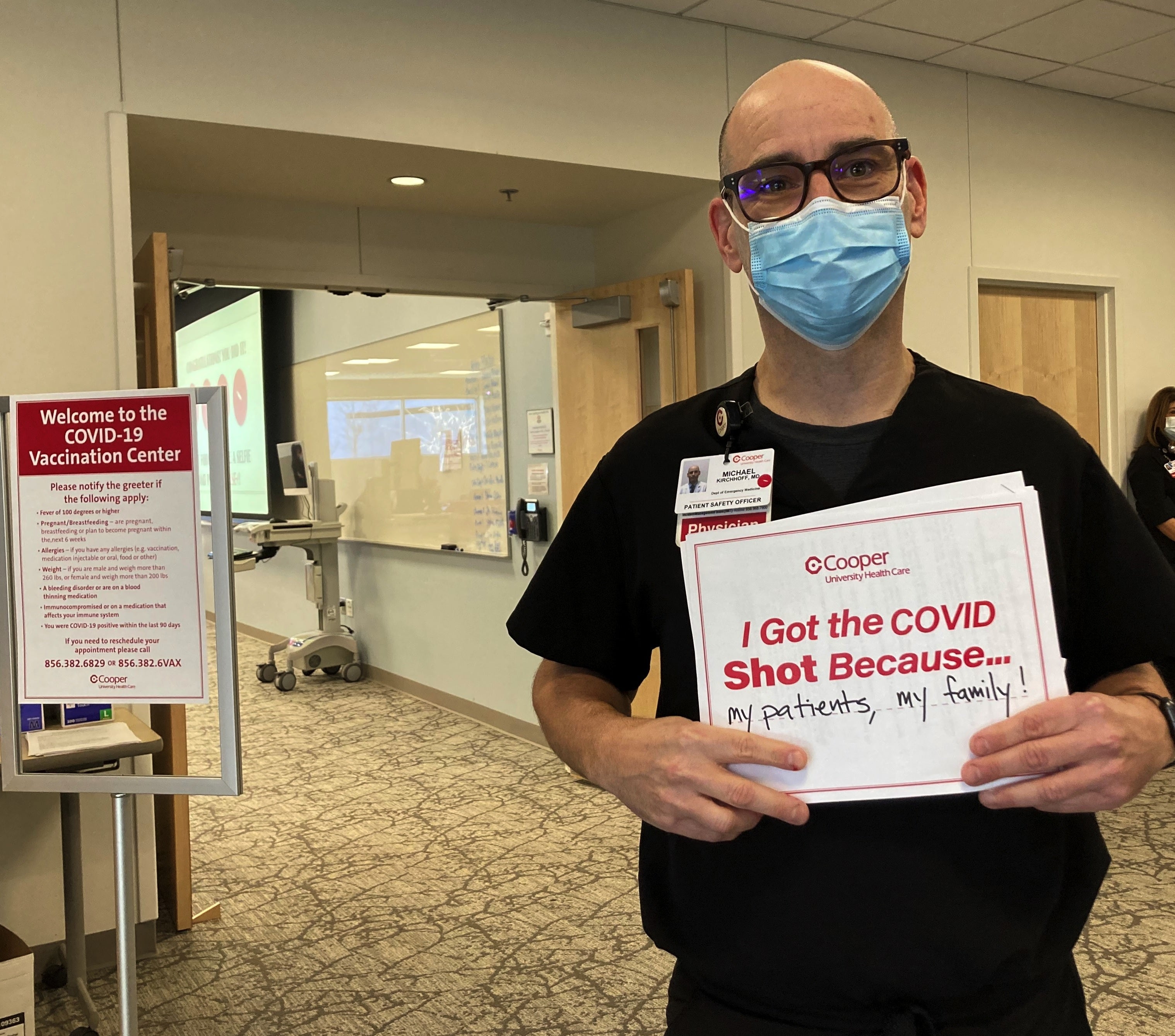
Kirchhoff stressed that despite the emotional experience, he knows the vaccine will not protect him and his patients completely. So he will keep wearing his protective equipment, and keep doing everything he is doing now to keep his patients and coworkers safe.
“Will I change anything when I go to work? No. Will I feel a little bit better? Yes, because I have yet another thing keeping me and my patients and my family safe.”
Robert Johnson
Dean of Rutgers New Jersey Medical School, director of the Division of Adolescent and Young Adult Medicine, Rutgers University
Robert Johnson and his wife love the theater. They enjoy dining at restaurants and traveling. Johnson is under no illusions that his first dose of the COVID-19 vaccine means he can do any of that again right away, but it’s one step in the right direction.
Johnson is part of a team that has tested and treated hundreds of patients for COVID-19, and in his own clinical practice he has also taken care of teens and young adults with the virus. In addition, the physician is at high-risk as an African American and a 74-year-old.

He spoke to WHYY after receiving his first shot.
“This morning, it makes me feel different; I’m not less cautious, but less concerned about running into somebody who is infected and getting infected myself,” he said.
“I’ve made that discovery a number of times, where a patient comes in and wasn’t sick, but had infections, and I had reason to worry,” he said. “I still have reason to worry, because I’m not immune yet, but I now know there is an end to this problem.”

Get daily updates from WHYY News!
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.



![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)






