High temps can make people with dementia irritable, confused, and uncomfortable. What to know
People with Alzheimer’s disease or other conditions that cause cognitive decline can struggle to say they are hot during extreme heat, so caregivers must watch for changes.

Alice “Candy” Loughney, 71, has Alzheimer’s disease and moved into a long-term care facility in Monroeville after her symptoms became too much for her husband to manage. (Quinn Glabicki / for Spotlight PA & PublicSource)
This story originally appeared on Spotlight PA.
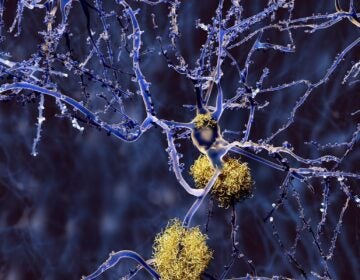
People with dementia are more vulnerable to the summer heat. Studies show that when temperatures climb, people are more likely to die or be admitted to the hospital if they have Alzheimer’s disease, or another neurological condition that causes cognitive decline.
Sometimes, the signs that someone with dementia needs help are obvious, said Sara Murphy, vice president of programs and services for the Alzheimer’s Association’s Greater Pennsylvania Chapter. For example, an older person might be wearing a fur coat in 90-degree weather. At other times, the signals are subtle, and caregivers have to be vigilant to ensure someone’s comfort and safety.
Additionally, because diseases like Alzheimer’s, Parkinson’s, and Lewy body dementia are progressive, the physical and mental abilities of people with these types of diagnoses can constantly change, which means caregivers must always be on their toes.
In this interview, which has been condensed for clarity and length, Murphy told Spotlight PA that during hot weather, caregivers for people with dementia should pay close attention to patients’ emotional and physical states and think like detectives.
Spotlight PA: Are there physiological reasons why a person with Alzheimer’s might be more vulnerable to heat?
Sara Murphy: For the average Joe who doesn’t have any cognitive impairment, they’re able to regulate temperature and realize that it’s really hot and to dress appropriately.
But with someone with any type of dementia, it can affect the person’s ability to regulate their body temperature and their perception of temperature changes. So then that can make the person with dementia more sensitive to hot and cold conditions, but also difficult for them to take appropriate action.
They might be uncomfortable, but they might not be able to convey that they’re hot. Instead, you might see behavior changes, like someone could be more irritable … because they’re too hot, but they might not be able to express that.
You just mentioned that someone experiencing discomfort due to the heat can act a little irritable. Are there other signs that a caregiver should be looking out for?
So you might see physical things like lightheadedness, dizziness, gait. If they are dehydrated, they might have dry mouth, and difficulty sleeping because someone with Alzheimer’s or dementia, they might not know how to adjust the air conditioning or the blanket. If you’re not getting enough sleep because you are too hot then that’s going to cause increased irritability, agitation, but also confusion.
But going back to the signs of dehydration, dark urine is obviously an indicator as well. And then you might see a decrease in actually going to the bathroom; that’s another sign that they probably aren’t getting enough water. And depending on the medication, they may not sweat as much, so as a result of that they could have muscle cramps.
It sounds like caregivers have to be really observant.
Absolutely. It’s almost like they’re detectives. They’re the problem solvers. They’re figuring out, “OK, what is triggering this new behavior?” For example, maybe someone has fallen in their home, and maybe it was because they were lightheaded, due to overheating and the room didn’t have air conditioning.
Because of the disease processes with Alzheimer’s and dementia, what’s actually happening is that you’re losing those brain cells that are giving the average Joe the ability to make good judgments, to think, to plan, to reason, or to execute on something.
I also want to talk about the danger of wandering, which is when someone leaves their location because they feel lost or confused. Wandering is a common symptom of dementia and when there’s dangerous weather, it makes wandering even more dangerous. So, what should a caregiver do to prevent wandering?
I do feel that having a neighbor or someone who lives close by and who can be on the lookout is important.
Also, some folks have GPS devices to keep an eye on someone if they are in fear that they might wander off. Safety-proofing near the exit doors is another strategy, as well as childproofing the doorknobs.
A lot of times we do see wandering towards the end of the day, and we see that increase of confusion, agitation. And so being mindful of any changes in someone’s environment that could spark them wanting to leave.
Also, if you start to hear someone with some form of dementia say, “I want to go home,” or “I’m wanting to see someone who is deceased,” that could help the caregiver know that there’s loneliness, there’s isolation, and that’s another trigger.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.