Delaware legislators attempt to expand medicinal marijuana eligibility
Listen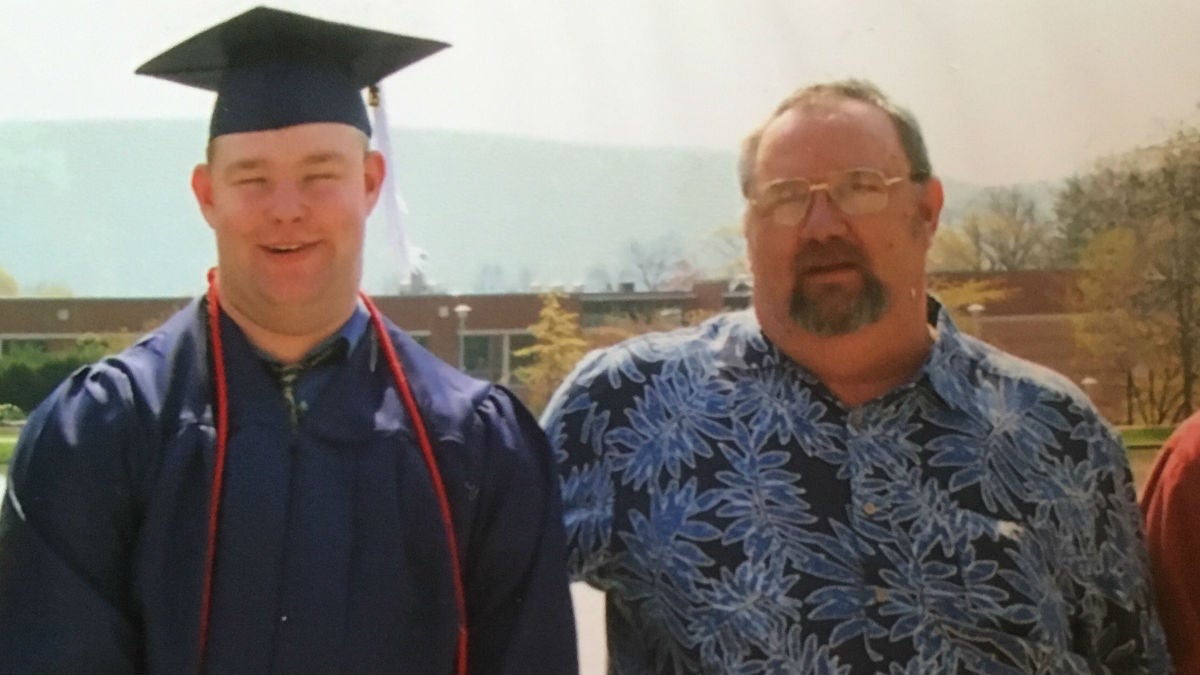
Rich Jester and his father
A new bill aims to broaden support for suffering Delawareans who could benefit from medicinal marijuana.
After he was diagnosed with stage 3 lung cancer in 2014, Rich Jester’s father, Robert, began chemotherapy and radiation treatment. As a result of the treatments, Robert began to feel common symptoms—lethargy, constipation, vomiting, diarrhea, inability to sleep and lack of appetite.
Jester, a licensed care giver whose wife uses medicinal marijuana for fibromyalgia, chronic pain and nausea, suggested medicinal marijuana to his ailing father.
“I made one of the most difficult conversations a son has to make to an extremely conservative dad,” he said. “I was fully prepared for my father to disown me—but he didn’t.”
Jester said he noticed drastic improvements to his father’s well-being after taking the medication in oil form.
“Before cannabis oil my dad never got out of bed,” he said. “After cannabis oil my father was always downstairs, or in the kitchen, or up or outside.”
After a while, Jester’s father chose to get permission from his doctor to receive medicinal marijuana legally. Jester said the doctor refused, and threatened to discontinue treatment and report him and his wife to authorities if he continued to take the oil.
His father stopped and Jester saw a rapid decline.
“My dad hadn’t eaten for 28 days until he died,” Jester said. “I would have killed to give him anything, get him to eat a cookie, get him to eat some THC oil. Anything to see him eat something and he didn’t want to get my mom arrested, so he wouldn’t do it.”
Jester is one of several Delawareans who have witnessed the medicinal benefits of marijuana, and one of many residents who say they’ve faced difficulty receiving approval from their doctor.
“We have anecdotal evidence of medical marijuana being effective, yet we also know—and I’ve also spoken to a constituent who has cancer and it drove her nuts she either had to be a criminal and break the law in the state or be able to avoid the kind of narcotic pain medicine typically prescribed,” said State Rep. Paul Baumbach, D-Newark.
Medicinal marijuana is legal for individuals with certain illnesses. But Baumbach, who met Jester after he wrote a petition, hopes to expand that list of qualifications to more Delawareans so they won’t have experiences like Jester’s.
Baumbach has introduced a bi-partisan bill that, if passed, would qualify terminally ill patients of all ages to receive medicinal marijuana to treat pain, anxiety and depression caused by their illness or supporting treatments.
Pro-medicinal marijuana residents support the bill, but still are concerned doctors aren’t educated on the medicine or simply won’t sign off on it due to their personal beliefs.
The legislation known as “Bob’s Bill,” after Jester’s father, builds upon the Delaware Medical Marijuana Act and “Rylie’s Law,” and has several other sponsors.
Since July 2012 Delawareans over 18 have been able to receive doctor-recommended medicinal marijuana with a state-issued ID.
If a doctor concludes their patient has one of the qualifying conditions they can sign off on the ID, and then the patient can take the ID to the state-run dispensary in Wilmington to receive the medication.
The Division of Public Health, which oversees the First State Compassion Center dispensary, plans to complete contract negotiations for two new centers in Kent and Sussex counties by the end of summer.
There are several current qualifying conditions for adults, including cancer, HIV/AIDS and intractable epilepsy.
Last year, Sen. Ernie Lopez, R-Lewes, introduced legislation that expanded the use of medical marijuana oil to those under 18, if they have intractable epilepsy and certain muscle disorders. The legislation known as “Rylie’s Law” passed in the Senate and the House almost unanimously with one legislator absent.
Medicinal marijuana experts say oils do not cause the consumer to become high, and are a safe option for children with various medical conditions.
“Riley’s law was one of the most important pieces of legislation to go through the general assembly in 2015 because the moment the governor signed… (individuals) immediately began to have access to the medication without threat of legal harm to the family,” said Lopez, who also is sponsoring Baumbach’s bill.
In 2013, Rylie, now 10, was diagnosed with aggressive giant cell granuloma, which are bone consuming tumors in the face. Two weeks after undergoing a seven-hour surgery she began having episodes that were later diagnosed as seizures. The medications she received caused severe mood changes, depression and bone pain.
While researching treatment options, Rylie’s mother Janie Maedler learned about cannabis oil. She joined a support group and Rylie began using it not long after her surgery.
After using the treatment, Maedler said her daughter made major improvements. She then started to slowly ween her off the drug, but her seizures became worse. That’s when she contacted Lopez in an effort to legalize the oil for those under 18.
“Once the law passed she was able to get on the real cannabis medication. She has been doing remarkable,” Maedler said. “She gets straight A’s, she never gets sick.”
Lopez is now trying to dispose of any barriers to the medication for those who need it. Senate Bill 181, introduced a couple months ago, would allow for minors with the prescribed medical card to have access to cannabis oils on school property.
“If they’re in school the majority of the day and there’s a time their dosage needs to occur during school hours the student has to leave school to take that medicine, and that’s not fair,” Lopez said.
In the meantime, Baumbach hopes to expand the current law to children and adults who are terminally ill, which would be defined as any disease, illness or condition sustained by a person deemed fatal within a year regardless of any other medical treatment. Children would still be limited to cannabis oils.
“It’s just another example of collaborative bi-partisan work in regards to a quality of life issue, and that was something I felt was more than reasonable,” Lopez said. “Someone who is terminally ill should have access to legal, healthy, scientifically proven medication that improves their quality of life for the end of life.”
Maedler said she believes expanding eligibility to children who are terminally ill is necessary.
“To be able to use cannabis in a way to improve quality of life in those last times and minimize that torture they’re going through in the last stage of life…with the proper guidance and the proper doses children can get through those end of life events with cognitive ability and share some moments with their family before they leave,” she said.
Maedler added she believes cannabis oil should be used in addition to chemotherapy and radiation as a supplement, rather than a replacement.
According to the Division of Public Health there currently are 1,550 card holders in the state, and it expects an increase. Currently only 0.3 percent of Delawareans under 18 hold the ID card. The largest percentage, 28.3 percent, are between the ages of 51 and 60. The majority of card holders use the medication for pain—use for muscle spasms falls second and cancer falls third in line.
Emily Knearl of DPH said in a statement the department has not had the opportunity to comprehensively review Baumbach’s proposal.
“We look forward to discussing it with him, the medical community and other stakeholders,” she said. “We would not anticipate any difficulty fulfilling additional demand.”
Cynthia Ferguson, the Director of Delaware NORML, an organization advocating for the legalization of marijuana, said she supports Baumbach’s legislation.
“There are a lot of studies that show it does help with anxiety, depression, and also a lot of this is for end of life stuff and at the end of your life you should enjoy it,” said Ferguson, a recreational user who later learned of marijuana’s healing qualities.
“There’s no legislation out there that says, ‘You can’t prescribe kids oxycodone or Percocet,’ even though these things are proven to cause addiction and from the addiction comes heroin. Yet we have to do legislation for a drug that has a less addictive rate and is nontoxic.”
Debra McPherson-Nau, executive director of the Delaware Patient Network, said there are a couple different types of oils available. CBD oils are helpful for children because there are no psychoactive effects. Rick Simpson oils, she said, are more potent and better for adults.
“Believe it or not, it’s less harmful but more potent than prescription drugs,” McPherson-Nau said. “There are a number of children using the oil in Delaware and their parents thank the oil for saving their lives.”
But she said many doctors in Delaware won’t sign off on the medication, even if the patient is a qualified candidate. McPherson-Nau said she too has faced challenges getting her doctor to renew her prescription.
“Having a law in place with oils available for children and adults is really nice, but try to find a doctor to sign off on it—that’s where the difficulty is,” she said.
McPherson-Nau said that’s one of the reasons she started the Delaware Patient Network—to educate the public and provide support to patients.
“A lot of people think it’s just a bunch of hippies sitting around looking for an excuse to get it legal,” she said.
Maedler said Riley had to leave her original doctor because she refused to sign off on the medication.
“Instead of trying to diagnose my daughter she blamed it on the oil and we were looking for answers and we weren’t getting any answers as to why these seizures were happening,” she said.
Maedler said she is very happy with Rylie’s current doctor, and also visits a neurologist in South Carolina who supports using the medication. She said Riley has 90 percent seizure control on the oils alone, and she just started taking seizure medication on a low dose to try to get to 100 percent.
Nancy Lemus said her son Christopher, now 10, also has felt the benefits of using cannabis oil. Christopher has cerebral palsy, which causes tightness in his body, and has a movement disorder known as Dystonia that causes severe muscle spasms, for which he is prescribed narcotics. This year he received a trachea in order to breathe properly. Christopher began using oil products in October.
“Christopher is able to enjoy his life, he started going back to school, he could stay awake, and he’s really enjoying his life as a 10-year-old,” Lemus said. “He’s not over medicated, which was one of the biggest concerns we had. With cannabis he’s still on traditional narcotics, but he does not have to be over dosed.”
However, she said she still faces conflicts with doctors who are cautious about the medication. Lemus said her doctor would not help them with any medication that came from the dispensary, which meant she had no choice but to receive oil at home from Colorado.
She also said when Christopher was in the hospital the staff couldn’t apply the oil, so he had to be discharged so he could receive the treatment at home.
“Right now I feel like our state is not providing medical professionals with any education because even when I want to talk about it some doctors will dismiss the conversation and want nothing to do with it,” Lemus said.
Baumbach said he and the other legislators are aware of some of the negative consequences, which is why there are tighter restrictions on juveniles.
“We’re very receptive to the potential impact of marijuana on youth and brain development. That’s one of the reasons it’s very limited for minors,” Baumbach said.
“When looking at terminal illness we said, ‘Well what about youth? Is there some reason we would prohibit them and for the terminally ill?’ No.”
Dr. John Goodill, a palliative care physician, said the problem with medicinal marijuana is, because it’s an illegal substance, there isn’t a lot of research on it. Most physicians don’t know how to dose it, and there’s no regulation of the substance itself for quantity or quality, or whether there are other impurities mixed in with the product, he said.
“I think our experience is limited as far as good quality, evidence-based. A lot of it is being anecdotally used right now,” Goodill said. “But in advanced complex pain situations it can be helpful in some people, and some people (for) appetite and nausea.”
He said if one of his patients asked about medicinal marijuana he would help them weigh the risks and benefits. Smoking it has negative effects on the lungs, and also can cause problems with patients who have mental illness, and it can make depression worse, Goodill said. But he said he would be open to supporting their use if it benefited them.
“I think it is not going away, and I think there ought to be more research done to determine when it is useful and when it is not so we can appropriately inform the public. And physicians should be part of that process and have a better grasp of its usefulness as a therapeutic substance,” Goodill said.
He said he believes one of the reasons there hasn’t been enough research and education is because the federal government labels it a schedule one drug, along with drugs like heroin and meth.
“Doctors are people and they live in society, and you know there are people that have opinions on social drugs like marijuana. And I think some physicians are more open to the possibility there may be reasonable therapeutic effects of the substance and others would rather not be involved in it,” Goodill said.
Jester said he hopes by expanding the qualifications more doctors will become educated, and more individuals will be able to live the end of their life more fully.
“When you’re terminally ill you have few choices in life and you should be allowed to choose how you spend your last days,” he said.
“Cannabis can alleviate the pain without taking your loved ones away from you, and at a time in your life when every minute, every hour, every conversation you have with that person could be the last one, the more they can be coherent, the more they can be lucid and the more they can be not over medicated the more you’re going to remember that time.”
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.





