Delaware hospitals have fewer and fewer COVID-19 patients
Public health officials and hospitals had feared disaster in the spring. But the number of people needing inpatient treatment has steadily declined.
Listen 1:46
Dr. Mike Benninghoff confers with registered nurse Lea Robbins in Christiana Hospital's intensive care unit for COVID-19 patients. (Courtesy of ChristianaCare)
Are you on the front lines of the coronavirus? Help us report on the pandemic.
Toward the end of April, with the coronavirus spreading rapidly throughout Delaware, hospitals, public health officials and emergency planners prepared for a doomsday scenario.
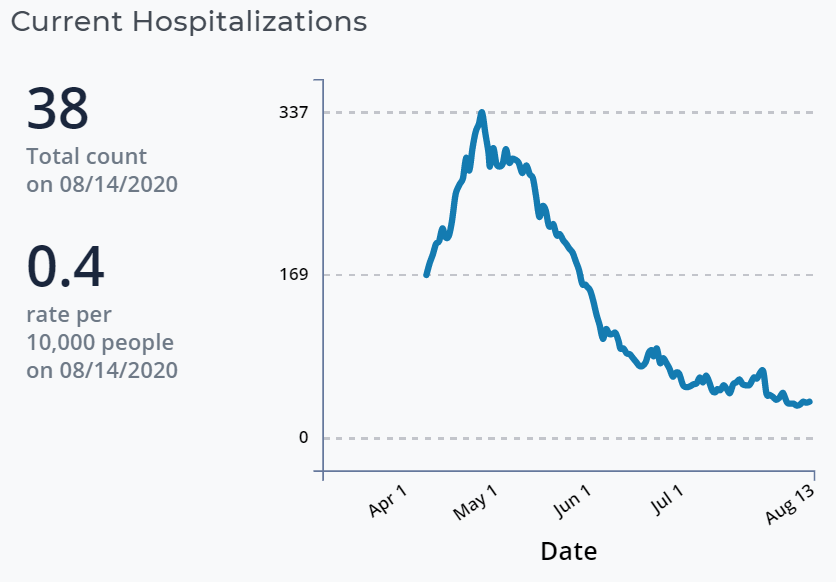
One day brought 458 newly confirmed cases. There were as many 337 people in hospitals statewide, 71 of them in critical condition. The disease was ravaging nursing homes.
Fearing that hospitals and their intensive care units would be overwhelmed by a flood of gravely ill and dying patients, health care officials and the National Guard set up two alternate hospitals and made plans for a third.
It didn’t happen.
Though cases have continued to rise throughout the spring and summer at a steady pace, with 16,340 total cases and 593 related deaths, the burden on hospitals steadily waned, and the flood has become barely a trickle.
Put another way, few COVID-19 patients in Delaware are sick enough to be admitted to the hospital.

The number of people hospitalized fell below 100 on June 12 and has steadily continued to fall. As of Friday, the state reported that 38 people are getting inpatient treatment. Ten are in critical condition.
“We’re not seeing the level of severe disease we saw early in the pandemic,’’ Dr. Rick Pescatore, chief physician at the state Division of Public Health, told WHYY News.
Average daily hospitalizations is just one of the three factors Gov. John Carney is monitoring to qualify for a full Phase 3 economic reopening and in-classroom K-12 learning. The other two factors — percentage of positive tests, now at 4.2%, and number of daily cases, now at 53 — are still too high to qualify for a move from Phase 2 to Phase 3, Carney has repeatedly said.
Pescatore credits the plummet in hospitalizations to:
- Rules mandating physical distancing, face coverings, smaller gatherings and other measures he calls the “legs of the infection prevention tool’’ that aim to stem spread of the virus, especially among the elderly population with underlying health conditions.
- Increased knowledge of the disease by the medical community, which has led to more effective pharmaceutical and non-pharmaceutical interventions.
- Increased prevalence of cases among younger, healthier people, many of whom only get minor symptoms.
People under the age of 35 account for 39% of Delaware’s total case count but only 2% of deaths, public health records show. The state does not collect data from hospitals for coronavirus admissions by age.
Pescatore, who has moonlighted as an emergency room physician in Pennsylvania, New Jersey and New York during the pandemic, said the medical community has learned better strategies for handling COVID-19 cases without admitting patients to the hospital.
“We know better how to intervene upon it and what to expect from a clinical trajectory, but there also clearly have been fundamental changes in how we approach it, how the virus affects different populations,” Pescatore said.
One effective method is what Pescatore called “pulmonary toileting” and is also known as “pulmonary hygiene.” Patients can do exercises and use other procedures that help clear mucus from their airways so their lungs get enough oxygen and their respiratory systems work more efficiently.
Doctors can also prescribe medications to help with fever, cough and pain management, Pescatore said.
Enhanced knowledge has “bridged the gap between patients and physicians,” he said. “I think we’re seeing a better uptick in the community of self-care at home.”

‘We have to think about what’s to come’
Pescatore and Dr. Mike Benninghoff, who heads intensive care at ChristianaCare, the state’s largest hospital system, aren’t proclaiming victory, though.
With no vaccine approved yet, they warn that with the fall flu season fast approaching and a resurgence of the pandemic predicted, hospital beds and ICU units could again fill up rapidly.
“I’m more worried about the flu because the flu looks just like COVID-19,” Benninghoff said. “All these viral pneumonias look very familiar, and I’m concerned that there’s gonna be some kind of cross-pollination, perhaps not just coronavirus getting worse as they reopen things, whether it be college, high school, or they allow people to gather in a larger fashion.”
If people stop practicing physical distancing and wearing masks or “aren’t using common sense,’’ Benninghoff said, “then absolutely, because of the asymptomatic carrier stage, it could spread through a whole group of people really fast.”
Benninghoff said he’s constantly reviewing hospital admissions for COVID-19 “to prepare for what may be inevitable. So we have our guard up there.”
Pescatore agreed.
“This is not over. And we still have a ton to learn, just like we learn so much every week, every single day,’’ he said. “We are fortunate that we have very much flattened the curve here in Delaware.
“But we need to remain vigilant because there’s much that we still don’t know. We have to think about what’s to come.”

Get daily updates from WHYY News!
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.



![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)


