Sickle cell cures are near, but some adults worry inadequate care could make them ineligible
Care for adults with sickle cell disease has lagged behind pediatric care. Some adults may not be well enough to receive cures when they come.
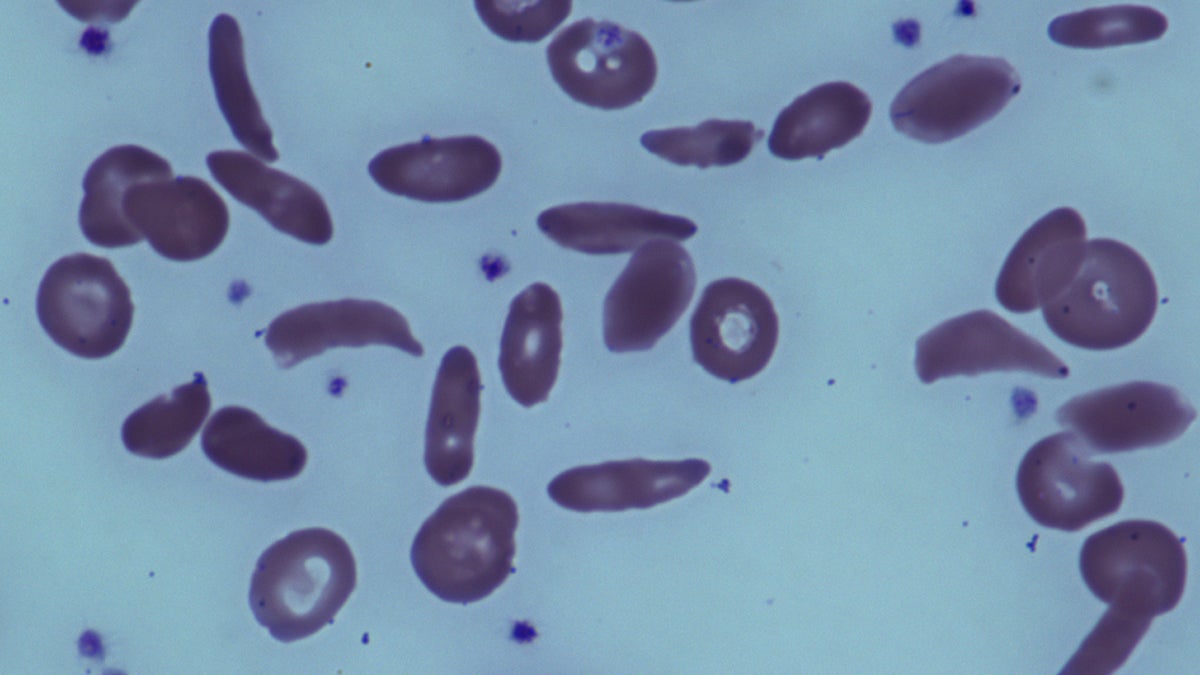
This June 2014 image provided by the National Institutes of Health, shows red blood cells in a patient with sickle cell disease at the National Institutes of Health Clinical Center in Bethesda, Md. A small but promising government study by National Institutes of Health found that bone marrow transplants can reverse severe sickle cell disease in adults. Results were published Tuesday, July 1, 2014, in the Journal of the American Medical Association. (AP Photo/National Institutes of Health)
Tahirah Austin vividly remembers the day she was diagnosed with sickle cell disease. She was 6 years old.
She went to the school nurse with intense stomach pain, so bad that when her father came to pick her up, he immediately rushed her to Children’s Hospital of Philadelphia. She went through numerous tests, while the doctors conferred. Was it cancer? Something else?
Eventually, pediatric hematologist Kim Smith-Whitley determined what it was.
“I knew whatever was going on was very serious,” said Austin, who is now 32. “And I can remember Dr. Smith-Whitley being there and hearing the term sickle cell disease, not knowing what it meant yet, and not really understanding what was going on, but I knew I was really sick.”
Sickle cell disease is a genetic, inherited condition, affecting primarily those of African and Middle Eastern descent. More than 1,000 Philadelphians have the disease, which affects 70,000 to 100,000 people nationally.
A mutation in the gene for hemoglobin causes red blood cells to form rigid, crescent shapes, which clog blood vessels and prevent blood and oxygen from getting to certain organs. If it involves a bone or certain muscles, it can cause pain. If the condition affects the lungs, it can cause a pneumonia-like condition called acute chest syndrome. If the warped cells clog blood vessels in the brain, it can cause a stroke.
Historically, only about 40% of patients made it to 20, due to the sustained organ damage that eventually led to a deadly stroke or acute chest syndrome episode.
Now, however, 92% of those with sickle cell live to 20, and many live into their 40s and 50s. Infant screening identifies those with sickle cell at birth and immediately puts them on antibiotics to ward off deadly chest infections and other complications.
Even more promising, there are now cures on the very near horizon, ranging from gene therapies such as those being developed in Stefano Rivella’s lab at CHOP, to therapies using the gene-editing technology CRISPR.
But Austin, now married with a 2-year-old daughter, worries she may not be eligible for those cures if she doesn’t continue to get adequate care as an adult, something that until now has been a challenge.
“A lot of the resources that are out there are geared towards pediatrics,” she said, “and the adult community is usually left out on a whim, having nothing.”
When treatment is hard to find
Sickle cell is often still thought of as a pediatric disease, and with many sickle cell patients on Medicaid, which has lower reimbursement rates, many hematologists caring for adults do not specialize in its treatment.
That means many adults end up using the emergency room in a pain crisis, which brings with it the stereotypes that accompany a predominantly black population who come to the ER asking for specific and very strong pain medications like morphine and Dilaudid.
“That’s when somebody is going to question, well, does this person really have sickle cell disease or not?” said Smith-Whitley, Austin’s childhood doctor, who now runs CHOP’s Comprehensive Sickle Cell Center. “And why is this person so knowledgeable about their opioids? And that raises a red flag.”
That, in turn, sours a patient’s record, even though the supposed red flag is often based not on improper behavior but instead on a racist stereotype.
“Now you’re seen as being a drug seeker, even if you aren’t,” Austin said. “You just haven’t found a medical home.”
Eventually, Smith-Whitley said, many patients give up.
“Because of the way individuals with sickle cell have been treated in … emergency room settings,” Smith-Whitley said, “they are reluctant to go there when they have pain, so they wait and they wait and they wait, and they try to treat this at home.”
Depending on what complications arise, that can lead to further organ damage or even death. Smith-Whitley said that not only poses an immediate threat to patients — it also decreases the odds they will be eligible for breakthrough treatments when they become available because their organs will be too compromised to sustain intense protocols that often involve chemotherapy to make them effective.
“Every organ is impacted by sickle cell disease,” she said. “So how do we keep that individual healthy enough so that when curative therapies are available, they’re healthy enough to receive them?”

Austin stayed with CHOP until she was 23, far older than a typical pediatric patient, because she couldn’t find a doctor who provided adult sickle cell care at the same level she’d received as a child. And even once she found a doctor she liked, he mysteriously quit last year, leaving her -— and hundreds of other sickle cell patients — without a medical home, only underscoring the fragility of the care network for adults.
Special programs emerge
She recently landed at the Hospital of the University of Pennsylvania, which about a year ago launched a Comprehensive Sickle Cell Program. The program, run by hematologist Farzana Sayani, is composed of a team of hematologists, nurses, social workers, mental health workers, and others, who can address the many health and psychosocial issues that arise from living with a chronic disease.
A similar program exists at Jefferson, and Sayani said the medical community in Philadelphia is getting better at addressing the needs of the adult sickle cell population.
“It has been slow to come,” she said. “But I think that … as our patients are living longer, there’s clearly more push and more emphasis too for us to do better.”
Like Smith-Whitley, Sayani is focused on the issue of cures and keeping her patients healthy enough so that they are candidates for them. That means focusing not only on sickle cell and the associated complications, but also on the health risks that increase in all patients as they age.
“As our adult patients are living longer, it is more than just sickle cell that they suffer with,” she said. “We should still be doing the routine monitoring for cholesterol and reduction of risk factors for heart disease and monitoring for cancer.”
Adults with sickle cell also have to deal with all the other issues adults deal with in their lives — work, relationships, family, bills. Those can bring joy but also stress, which can be a trigger for a sickle cell crisis.
There aren’t many resources to guide adults with sickle cell through balancing those issues with their chronic disease, which is why Austin and some of her friends with sickle cell have started Crescent, a nonprofit meant to help sickle cell patients with, as Austin put it, “adulting.”
“Like all of the adult things that you have to do — how do you do this now with living with a chronic illness, and what resources [are] out there that we can link them to?” Austin said. “And on our end, how can we be, you know, those mentors that help them with navigating all this and doing it with them so that eventually they can do it themselves?”
For her part, Austin keeps healthy by boxing with a trainer, eating a balanced diet, and reducing the stresses in her life where she can — which, as the mother of a 2-year-old, isn’t always easy.
“With being a mom and having a chronic illness, sometimes I want to be Superwoman because I felt like that for so long,” she said. “Now, it’s: Relax. Let someone else do it.”
Her daughter carries the sickle cell trait, but she doesn’t have the disease because Austin’s husband isn’t a carrier. Still, she knows that someday she’ll have to explain to her daughter what it means: that if she marries someone who is also a carrier, there is a 1-in-4 chance for each of her pregnancies that the baby will have sickle cell disease.
By then, Austin hopes, there might be a cure. But until that day comes, she said she will focus on taking care of herself and her family.
“I’m in a situation where I have to live healthier a lot longer for my daughter,” she said. ”It’s not just about me anymore.”
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.




