Pennsylvania doctors say mammograms could be used to detect early heart disease in women
Mammograms can detect the presence of breast arterial calcification, which is associated with a higher risk of future heart attacks and stroke.
Listen 1:11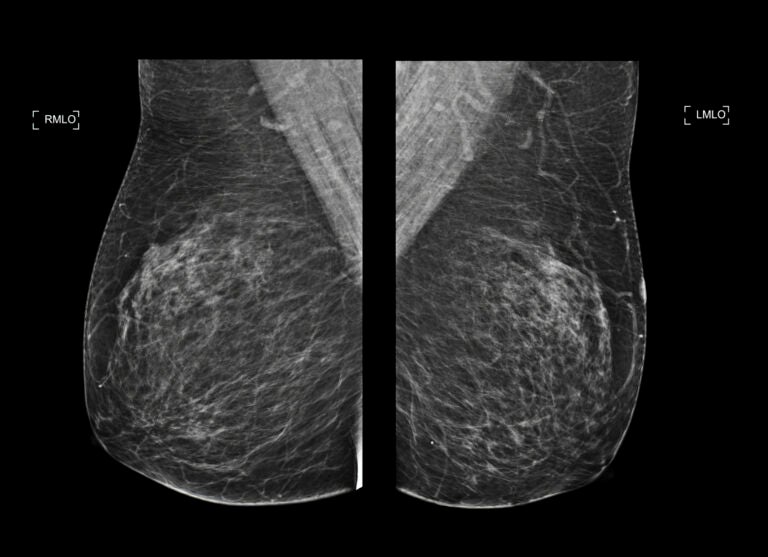
Mammograms detect tumors, but they can also identify calcifications in breast blood vessels – a sign of cardiovascular disease. (mr.suphachai praserdumrongchai/iStock)
From Philly and the Pa. suburbs to South Jersey and Delaware, what would you like WHYY News to cover? Let us know!
Mammograms are routinely recommended starting at age 40 to screen for breast cancer. But health care providers in the region are now using the imaging tests to check for another health risk factor: heart disease.
Specifically, they’re examining calcium buildup in the breast’s blood vessels, appearing as fine bright white lines or clusters on X-ray images. Previously, physicians and radiologists thought this buildup wasn’t associated with either breast cancer or cardiovascular disease.
“But the more recent research is showing that that’s not true,” said Dr. Matthew Nudy, a noninvasive cardiologist and assistant professor of medicine and public health science at Penn State College of Medicine.
Now, the evidence is clearer and stronger: the presence of calcium deposits in breast blood vessels, known as breast arterial calcification, or BAC, means a woman has a higher risk of heart attack, stroke or other cardiovascular complication as she gets older.
Nudy and other clinicians are hopeful that informing patients about their BAC levels could improve overall heart health among women and reduce serious and deadly cardiac events.
“If a patient knows that they have a BAC, they may be more in tune with what their blood pressure is, they may be more likely to get medications, they may be more aware of their health,” he said.
What to know about heart and breast health
Calcium buildup in heart arteries can cause blood vessels to narrow. That’s long been a sign of cardiovascular disease and heart attack risk.
Doctors can assess just how high the risk is by performing a coronary artery calcium scan, a type of noninvasive CT imaging. People with significant buildup are often encouraged to take medications like statins or make lifestyle changes through exercise, diet, sleep and other behaviors.
Similarly, mammograms can show calcium deposits in breast blood vessels. It’s a little different, Nudy said, as BAC causes vessels to become stiffer. But both narrow and stiff vessels are indicators of heart disease.
And many more women over the age of 40 have gotten a mammogram than a coronary artery calcium scan.
“It’s already being done for breast cancer screening across large numbers of patients in the population,” Nudy said. “So, it kind of overcomes the limitations of a coronary artery calcium scan.”
That’s one reason why Jefferson Health hospitals in the Greater Philadelphia area began adding BAC information on their mammogram screening reports last August.
A couple days before a woman is scheduled for a screening mammogram, patients get a flyer with information about BAC. It explains what it is, what the imaging tests and report may show, and what they could do with the results, including how to seek a full cardiovascular assessment.
It’s an educational moment as well as a warning, said Dr. Jason Shames, assistant professor of radiology at Thomas Jefferson University and associate director of research in the division of breast imaging at Jefferson Health.
“So that it’s not just a shock and awe, but it’s something that helps provide a positive impact for the patient without adding unnecessary stress and anxiety to an exam that’s already riddled with, unfortunately, a lot of anxiety and stress,” he said.
Radiologists review every breast cancer mammogram for BAC and let patients know whether it is present or not in the report they send out. Doctors can then help connect people to specialists and other heart-related care.
Jefferson, in partnership with Solis Mammography, also offers a program called Mammo+Heart, which takes it a step further by using artificial intelligence software to help analyze BAC visible in mammogram images to an even greater degree.
The program is an opt-in option as it comes at an additional cost to cover the added time and resources it takes for the deeper analysis.
How to interpret BAC findings
The absence of BAC on a mammogram doesn’t mean that people should assume they’re not at any risk for heart disease and cardiac events, experts say. Other findings in their blood work, family history and other types of imaging tests can still indicate a risk.
But detecting BAC through mammograms could present a new opportunity for women to identify at least one early sign of heart disease.
“I think this is one of those pieces of information that is hopefully going to start the conversation,” Shames said. “And continue the conversation with their primary care team, with their other family members, too, to say, ‘Wow I’m 40, I’m 50 and I already have these changes inside my body.’”
The findings could encourage someone to make lifestyle changes or seek medication when they wouldn’t otherwise, he said.
As a researcher, Nudy said the next step is to study and gather data on how BAC notifications influence the way people make new preventative health care decisions regarding their heart health.
“Does that maybe increase statins? Does that maybe have patients lead a healthier lifestyle? Does that mean patients eat healthier or exercise more? Does it actually lead to less heart attacks, less stroke, and less death over time? That would be key,” he said.

Get daily updates from WHYY News!
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.