Flu vaccine required for many area health workers
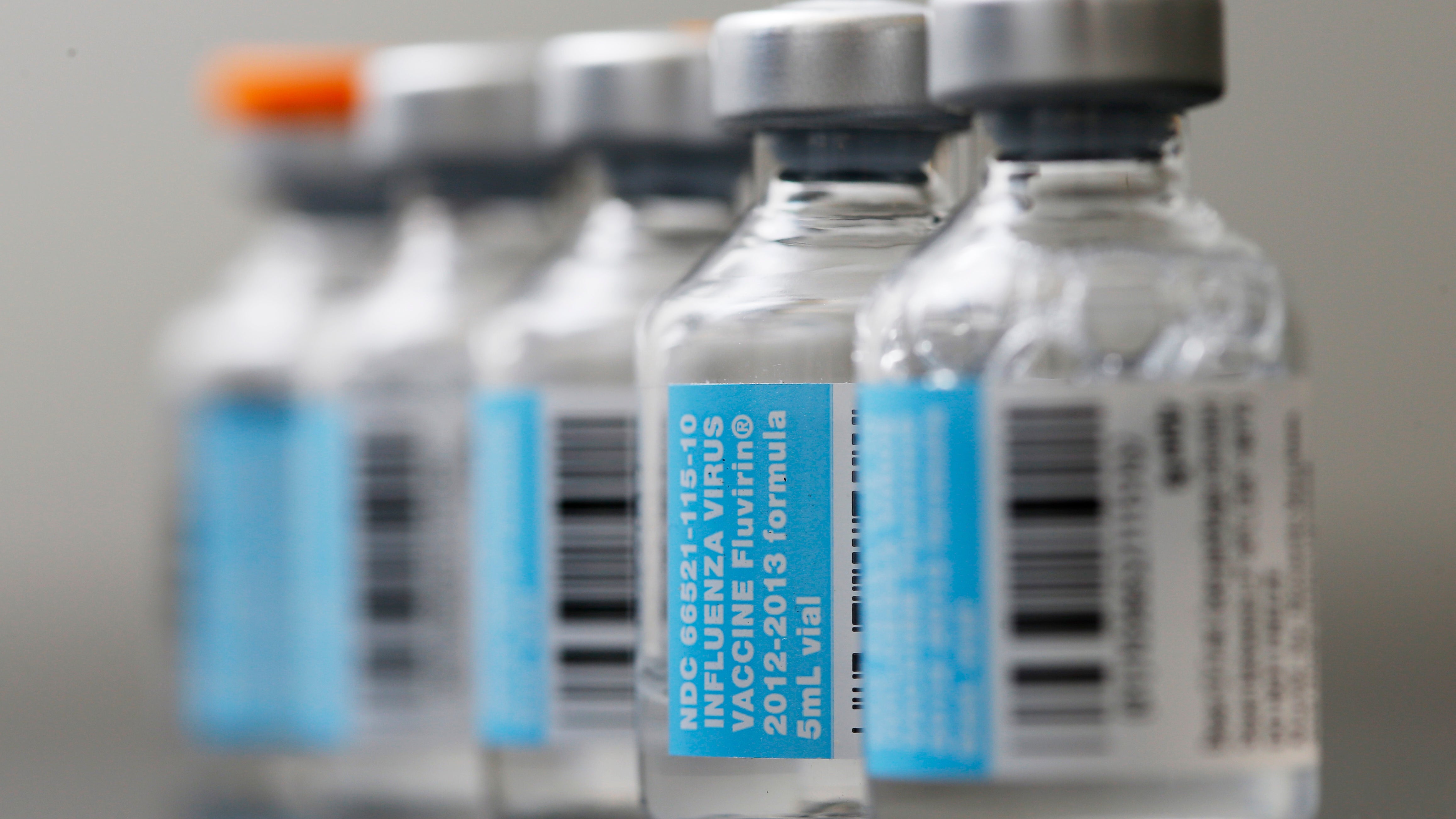
Vials of flu vaccine are displayed at Philly Flu Shots on Thursday, Jan. 10, 2013 in Philadelphia. The flu season arrived early in the U.S. this year, but health officials and experts say it's too early to say this will be a bad one. Experts say evidence so far is pointing to a moderate flu season - it just looks worse because last year's season was so mild. Flu usually doesn't blanket the country until late January or February. Now, it's already widespread in more than 40 states. (Matt Rourke/AP Photo)
As winter approaches, people may be weighing whether to get a flu vaccine. That is, unless you’re a health worker at one of at least two dozen hospitals around Philadelphia. Policies mandating that staff get vaccinated for the flu have taken greater hold in recent years, according to state health surveys.
One of the region’s earliest proponents is the University of Pennsylvania. And while it’s difficult to track the direct health impact of the policy, leaders there have been touting the pay-offs.
“We know that we have a lot of patients who are particularly vulnerable to complications from influenza – they’re more likely to get more sick, more likely to get pneumonia, even more likely to die,” says Dr. Amy Behrman, director of occupational medicine at the University of Pennsylvania. “And we were confident based on what’s known about influenza that we could reduce that risk – not completely, but significantly if we could improve that vaccine rate.”
So if enough people are vaccinated, they won’t get sick and spread the disease. Behrman says that’s important because nationwide, the flu causes upwards of 200,000 hospital admissions and anywhere from 3,000 to 50,000 deaths annually.
The hospital tried for years to improve vaccine rates through voluntary approaches, like making the vaccine easily and readily available. There were education campaigns. Even a cappella. But vaccine rates “hit a wall,” Behrman describes, of under 60 percent.
So in 2009, the hospital approved a policy mandating that everyone, with some religious and medical exemptions, get vaccinated. Behrman says the hospital has experienced a near 99 percent vaccination rate of its 18,000 workers each year since then.
“Somewhat paradoxically, I think that making the vaccine a norm – which is another way of thinking of it, it’s a normal thing to do – has actually to a larger extent reduced anxiety about the vaccine among our own population,” says Behrman. “Not entirely, but significantly.”
Behrman says no one has been fired over the policy; staff first get warnings if they don’t comply.
Skeptics of this approach, like Dr. Will Offry, a casualty nurse at Vancouver’s General Hospital, point to a lack of scientific evidence that vaccinating health care workers reduces flu transmission risks and questions whether that should override employee choice. Vaccine effectiveness varies by season, he wrote in a recent essay partnered with one by Behrman, and a majority of “influenza-like illness” come from other bacterial and viral pathogens, “none of which is prevented by seasonal influenza vaccines.”
Behrman says a combination of factors – like complimentary hand washing policies, seasonal flu variation, and difficulties tracking flu transmissions – make it hard to measure the full impact of Penn’s policy at this point, but she’s convinced it has contributed to “a noticeable drop-off” in hospital acquired flu infections, with neither of the hospital’s two identified cases directly traceable to a health care worker. Of the more than 40,000 immunizations done over three years, the hospital received eight medical complaints of systemic symptoms possibly related to the vaccine.
The Children’s Hospital of Philadelphia was another place to mandate vaccines early on in Philadelphia, and the policy has since spread. Chester County Hospital joined the ranks last year. Charlee Faucette, director of infection prevention at the hospital, says those hospitals’ examples helped with their own implementation.
“A lot of education, one-on-one coaching, and a lot of precedent helped us not have as difficult a time as thought we might,” says Faucette.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.

