Burning psychiatry’s bible: A new framework for diagnosing mental illness
Listen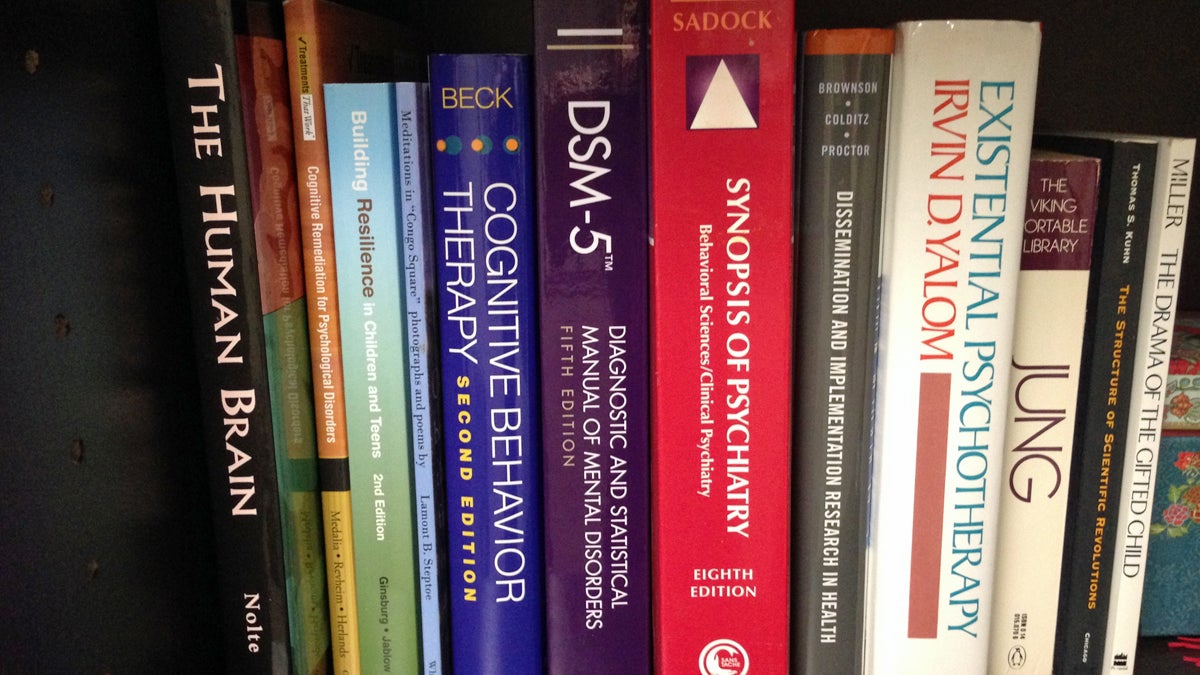
The Diagnostic and Statistical Manual of Mental Disorders
The National Institute of Mental Health is searching for a new director who will inherit a battle over how we think about afflictions of the mind.
Possibly the only thing scarier than public speaking, is getting called out while you’re public speaking. In the early 1990s, Judith Ford was a neuroscientist at Stanford. She’d made her name in studying the aging brain, but she’d just recently shifted to schizophrenia research. She was presenting at a conference in front of a room full of strangers.
“It was actually, probably, the first talk I’d ever given at a conference on schizophrenia,” she says. “And someone in the audience raised his hand, and said, ‘How can you study schizophrenia? Schizophrenia is just a composite of huge number of different kinds of symptoms, everything from hallucinations, to delusions, to thought disorder. How can you say anything about schizophrenia?’ And I really had no idea how to answer that.”
Ford says it was pretty traumatic. But she went back to her lab, and thought about what he had said. She hadn’t really been getting anywhere with her schizophrenia research, and by questioning the label of schizophrenia, he’d given her permission to move away from the framework of the Diagnostic and Statistical Manual of Mental Disorders, also known as the DSM.
“I decided that he was right,” she says. “Schizophrenia is a real wastebasket of symptoms. And I should focus on one. So, I decided, instead of studying schizophrenia, I would study auditory hallucinations.”
Auditory hallucinations are sounds made by a person’s own mind, that the person believes are coming from somewhere else. They’re one of the most common symptoms associated with a schizophrenia diagnosis.
“There are certain times,” Ford says, “when I can actually hear my mother saying things like, ‘If you just get your hair off your face you’d be such a pretty girl, Judy.’ You know, I can almost really hear her voice. But I do not believe that it is my mother speaking. I know that it is coming from inside my brain.”
“I think that it’s because I have a mechanism—and all animals on the planet have it—that enables us to know that what we are experiencing is a result of our own actions…and thoughts being a type of action. So it’s a way of tagging the experience as coming from self.”
Ford wants to figure out what that mechanism is. Because it seems to be weaker in people who have auditory hallucinations.
She now heads a lab at UC San Francisco. She studies auditory hallucinations using electroencephalogram testing, EEG. Our brain cells talk through small electrical impulses. So, she puts a cap full of electrodes on people’s heads that picks up that activity across the different regions of the person’s brain, and transmits it to a computer.
During the EEG test, she has people sit in a chair and make the “Ah” sound about a hundred times. She watches how their brain processes the sound when they’re actually making it. Then she plays back for them a recording of them making that sound.
Usually, with healthy control subjects, the hearing part of their brain doesn’t respond much to their own voice when they’re speaking. It’s really just interested in the recorded voice. But for people who have been diagnosed with schizophrenia, the hearing part of their brain still perks up when they’re the ones directly making the sound. It’s as if their brains don’t really distinguish between their voice on tape and their voice when they’re talking.
“Basically,” Ford says, “people with schizophrenia don’t tag these experiences as coming from self as readily as normal healthy people do.”
She says this extends even to the experience of touch. Other researchers have found that some people with schizophrenia actually can tickle themselves, they’re not discounting their own touch the way other people do.
For a long time this kind of brain research, focused on a particular symptom, didn’t really mesh with the way the National Institute of Mental Health was handing out research funding.
Bruce Cuthbert first came to the NIMH in 1998. He’d been studying mood disorders, and he says pretty much all the institute’s research back then was based around DSM-designated syndromes—schizophrenia, bipolar disorder, depression—each categorized by a framework of symptoms.
“And there were very simple-minded notions of diagnoses and how we measured outcomes,” he says. “In fact, I was so frustrated generally with what I thought was the poor quality of the science that after I’d been here seven years, I left.”
He started his own lab at the University of Minnesota. But the institute asked him back in 2009. Director Tom Insel was looking to change the way they directed research. The institute had begun to fear that by dividing up research by DSM categories, they were putting false limits on what people could study. Insel wanted a more science-based system for addressing mental illness.
“He invited me to return to the Institute,” Cuthbert says, “to lead this new effort that became called the Research Domain Criteria Project [RDoC]. It calls for studying human patients who may have DSM disorders, but we look at the disorders in the context of these basic functions and how they’re disrupted.”
It helps to think of RDoC as basically a giant grid. Listed down the side, you have all the different functions that can be disrupted by mental illness—memory, wakefulness, fear responses, etc.
And then, along the top of the grid, you have all the different factors that could impact those functions. Genes, brain circuitry, and behavior to name a few. The idea is to fill in the entire grid, so we can have a research-based understanding of the different types of functions at every possible level. That way, when we talk about, say, anxiety, we know we’re talking about something tied to a certain set of genes, a certain set of brain circuits, and behaviors.
Judith Ford, the auditory hallucination researcher, was at another conference, just a few years ago, when she ran into Bruce Cuthbert. He told her about the new RDoC system.
“We were standing out at one of those tall now-popular bar tables,” she remembers. “Just standing there chatting, and he told me about this, and I said, ‘Oh that’s fantastic! You know, this is how I think about it myself.’ And he said, ‘I know!’ because he knew what I was doing.”
She says RDoC gives her a grid to plug in what she was already doing, to a structure that had already been vetted by the NIMH.
Cuthbert points out that the origins of the DSM labels go back to the ancient Greeks, calling out afflictions like melancholia. Other syndromes like schizophrenia and bipolar disorder got classified in the 1800s.
“There really wasn’t any science at that time on which to base any diagnostic criteria,” he says. “They were forced like most of medicine at the time, to really go by symptoms.”
However, he still sees the DSM system as relevant.
“Well, it’s still the best understood way of describing mental disorders and all of the research up until the last five years ago or so has been done in terms of DSM disorders,” he reasons. “So all of our treatments have been worked out in terms of the DSM system.”
And many are not ready to let go of it.
In my reporting, I talked to about half a dozen different psychiatry researchers, most didn’t want to go on record with their concerns about RDoC. But the phrase that kept coming up was, “Don’t throw the baby out with the bathwater.” Sure, they said, there’re some flaws with the DSM system. But it gives us a common way to describe all the varieties of mental illnesses.
But Cuthbert says that fear’s mistaken. He’s now the acting director of the NIMH, and he says they’re not doing away with the DSM labels. They’re still using most of the terminology and they’re still funding research that uses the psychiatry bible.
“But that wide misunderstanding, I think, caused a lot of consternation in the field,” he says. “And we’ve been trying to clear up the messaging since then.”
Yes, he says, the National Institute of Mental Health is saying that the RDoC system has better science than the DSM. But the RDoC system’s not fully fleshed out yet. The grid it sets up still has a lot of holes in it.
Figuring out how to more fully make that bridge, from a system that’s well-established, the DSM, to a system that’s scientifically valid, the RDoC, will be the job of the next NIMH director.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.



