Fact check: The theory that SARS-CoV-2 is becoming milder
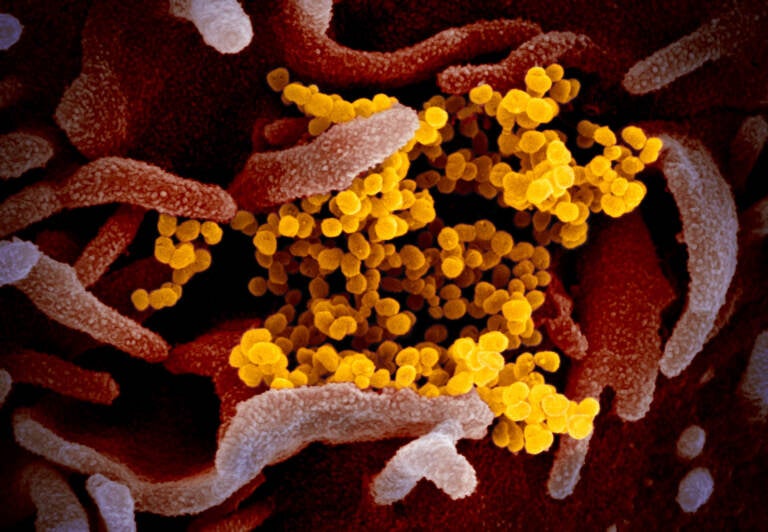
This colorized transmission electron micrograph (TEM) image shows SARS-CoV-2, also known as 2019-nCoV, the virus that causes COVID-19. This specimen was isolated from a patient in the U.S. Particles of the virus (yellow) are shown emerging from the surface of cells cultured in the lab (pink). The spikes on the outer edge of the virus particles give coronaviruses their name, meaning 'crown-like'.
There’s a growing narrative in the mainstream media, on social media — maybe even at your dinner table. That is: The coronavirus SARS-CoV-2 is weakening and evolving into a less deadly virus. In the future, each new variant that crops up will cause milder illness than the previous variant.
“There’s this story that we’re going to have variants that are progressively less severe,” says Dr. Roby Bhattacharyya, who’s an infectious disease specialist at Massachusetts General Hospital and Harvard Medical School.
But that’s completely untrue, Bhattacharyya says. “It’s comforting to think there might be some tendency for SARS-CoV-2 to evolve toward a milder form. That’s not what we’re seeing here.”
The origins of the mild theory
This narrative has arisen over the past month as scientists and doctors increasingly find evidence that the omicron variant of the coronavirus is less likely to cause severe disease than previous variants.
Data from hospitals in South Africa, the U.K., and the U.S. all suggest that the risk of a patient with omicron being admitted to a hospital is about half that observed with the delta variant. If you are admitted to the hospital, the risk of being put on a ventilator has dropped by about 75%.
On top of that, laboratory experiments and animal studies have shown that omicron acts differently in the lungs than previous variants. For example, biologists at the University of Cambridge found that omicron doesn’t infect lung cells as aggressively as delta does.
Specifically, Ravi Gupta and his team looked to see how well omicron and delta can infect lung and respiratory organoids — miniature 3D clusters of cells that resemble specific types of tissues in the lungs and respiratory tract. Omicron grew slower than delta — about a tenth as fast — inside the lung cells. But the team saw no difference in replication inside upper respiratory cells.
“Omicron’s growth was severely disabled in cells that delta infected very aggressively,” Gupta says. “And that was a real shock, because we were seeing omicron spreading very, very rapidly globally and yet omicron’s [ability to grow] in certain cell types was really attenuated.”
The team also found that omicron uses a different path to enter cells than delta. And this alternative entryway likely causes less damage inside the lungs. “I think these differences are having quite marked consequences in terms of what we’re seeing clinically,” Gupta says, “with patients having less inflammation in the lungs and a reduced requirement for supplemental oxygen.”
Gupta and his team published their findings online last month. And right away, the media “seized upon them as a sign of the endgame of COVID,” Gupta says. “I was very worried about that narrative because … omicron is still a very dangerous infection.”
And the emergence of a less severe variant like omicron is not a sign that SARS-CoV-2 is evolving into a milder virus that is less able to infect the lungs.
“It’s important to emphasize that the next variant — and there will definitely be one — may not evolve from omicron and it will not necessarily have these characteristics,” Gupta says.
An evolutionary history of SARS-CoV-2
Before omicron came along, SARS-CoV-2 was actually evolving to be more severe, says Bhattacharyya, of Harvard Medical School. “We’re looking at a virus that’s gotten progressively more severe over time,” he says.
A study from the U.K. found that alpha was about 40% more likely to kill a person than the original virus. And delta was about two times more likely to put you in the hospital than the alpha variant.
“Omicron may be a small step back in severity. But it’s probably more severe on its own than the original version of the virus,” Bhattacharyya says. Becoming “more mild” hasn’t been the trend or evolutionary trajectory, he says.
In addition, omicron didn’t evolve directly from delta. It evolved from an earlier version of the virus circulating in 2020. And so omicron could actually be more severe than its ancestral virus, and it could be progressing toward higher severity, Bhattacharyya says.
And thus, there’s no guarantee that the next variant to emerge will be milder. It could be the most severe yet.
“I think we don’t really know what direction this virus is taking,” says evolutionary biologist Stephen Goldstein at the University of Utah. “We’ve learned that trying to predict the evolutionary trajectory of this virus is very, very difficult. If not impossible.”
What will future COVID-19 surges look like?
When SARS-CoV-2 spreads from one person to another, that spread occurs primarily at the beginning of a person’s infection, even before they know they’re sick. During this period, the virus infects mainly the person’s upper respiratory tract. It hasn’t reached deep in the lungs, where severe disease occurs.
The primary way SARS-CoV-2 survives is by causing mild or moderate illness in the upper respiratory tract. “Causing severe illness is not one of SARS-CoV-2’s survival strategies, let’s say,” says Gupta, of the University of Cambridge.
So for a new variant to spread to more people and outcompete previous variants, it needs to become really good at infecting a person’s nose and airway. But it doesn’t matter how well the new variant infects cells in the deep lungs. As more people become immune to SARS-CoV-2, a new variant also has to be really good at evading antibodies and other immune responses.
So future variants will likely continue to improve their ability to infect and grow in the upper respiratory tract (and they will continue to be more immune evasive).
“Whether those changes also make the new variant more severe or less severe, that’s kind of the luck of the draw” Bhattacharyya says.
Why doom and gloom isn’t the only scenario
On the surface, this sounds horrible, right? It suggests that the next surge, after this omicron one, could be worse than even the delta surge.
But Goldstein says that’s probably not likely because there’s one more factor to take into account: people’s immunity.
Just as the virus is changing and evolving, so is your immune system. At the population level, immunity to SARS-CoV-2 is growing rapidly in the United States. More than half of the U.S. population has likely been infected. After the omicron surge, that percentage could rise above 80% or 90%. And more than 60% of people are vaccinated.
Both of those types of exposures to SARS-CoV-2 will reduce a person’s risk of severe disease in future surges, many studies have found. “Whether you’ve been previously infected or vaccinated, you’re more likely to have a milder course than a person who is immune naive,” Goldstein says.
And thus, over time, all future variants will likely look less severe than delta or earlier versions of the virus. “Even if the variant had no change in virulence, if the population now has a high level of existing immunity, then [the variant] will, in effect, be less virulent because the average severity of infections will go down over time,” he says.
So the hope among scientists is that no matter what the virus throws at us, future waves of COVID-19 will be less deadly and less disruptive, not because the virus itself has changed but because our bodies will be better able to handle the virus.
9(MDAzMzI1ODY3MDEyMzkzOTE3NjIxNDg3MQ001))