Can you reshape your brain’s response to pain?

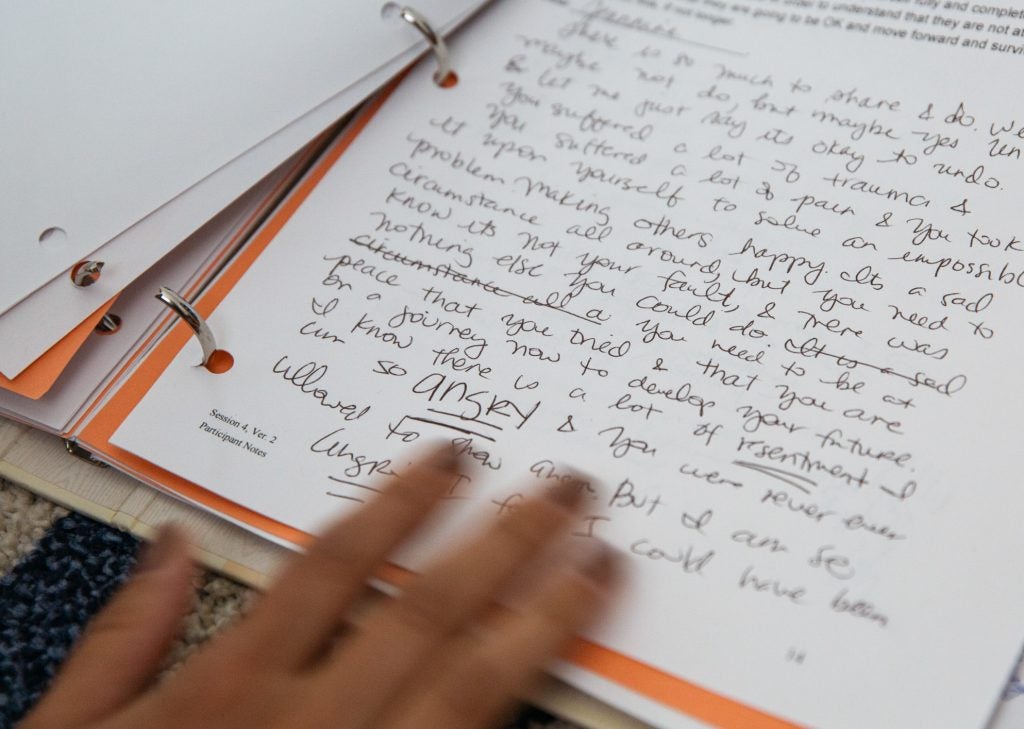
Jeannine sorts through a binder of writing assignments from her therapy. In keeping a journal about her past experiences with pain, she noticed that the pain symptoms began when she was around 8 — a time of escalating family trauma at home. (Jessica Pons for NPR)
Jeannine, who is 37 and lives in Burbank, Calif., has endured widespread pain since she was 8. She has been examined by dozens of doctors, but none of their X-rays, MRIs or other tests have turned up any evidence of physical injury or damage.
Over the years, desperate for relief, she tried changing her diet, wore belts to correct her posture and exercised to strengthen muscles. Taking lots of ibuprofen helped, she says, but doctors warned her that taking too much could cause gastric bleeding. Nothing else eased her discomfort. On a pain scale of 0 to 10, her pain ranged from “7 to 9, regularly,” she says.
Around 50 million Americans suffer from chronic pain. Most of us think of pain as something that arises after a physical injury, accident or damage from an illness or its treatment. But researchers are learning that, in some people, there can be another source of chronic pain.
Repeated exposure to psychological trauma, or deep anxiety or depression — especially in childhood — can leave a physical imprint on the brain that can make some people, like Jeannine, more vulnerable to chronic pain, scientists say. (We are not using her last name for reasons of privacy.)
Jeannine was eventually diagnosed with fibromyalgia — a condition characterized by widespread pain throughout the body, among other symptoms. The cause is unknown and likely varies from person to person.
The pain Jeannine experienced was physical. She’d feel “lightning bolts, kind of going up through my shoulders to my neck to my head,” she says. Other times, she’d suddenly experience the shooting pain of sciatica in her legs, and she often suffered from a “grinding pain” in her hips. “I would feel like I can’t walk anymore — it was just so very painful to walk.”
Then, about eight months ago, a friend suggested something else — emotional awareness and expression therapy.
Jeannine was skeptical. She’d periodically seen a counselor in “intensive therapy” over the years, and still, her terrible pain persisted.
But EAET, she learned from her clinical psychologist, Laura Payne, is a different sort of psychotherapy. It’s one of several behavioral therapies (among other interventions) included in a report from the U.S. Department of Health and Human Services titled “Pain Management Best Practices.” According to the report, published May 9, “Research indicates that EAET has a positive impact on pain intensity, pain interference, and depressive symptoms.”
EAET was developed in 2011 by psychologist Mark Lumley at Wayne State University and his colleague Dr. Howard Schubiner. It combines some techniques from traditional talk therapies (such as probing a patient’s life experience for insight and context) with those of cognitive behavioral therapy, which focuses more on skills training and changing harmful patterns of behavior.
It’s an emotion-focused treatment, Lumley says, aimed at helping people who are in widespread, medically unexplained pain.
In a 2017 study of patients with fibromyalgia, Lumley and his colleagues found that EAET decreased widespread pain and other related symptoms for some patients. “In summary,” the researchers concluded, “an intervention targeting emotional awareness and expression related to psychosocial adversity and conflict was well-received, more effective than a basic educational intervention, and had some advantages over CBT on pain.”
Lumley believes the treatment might also help patients who have other sorts of pain, though that’s yet to be proved.
So, how does it work?
For starters, as part of the therapy, Jeannine was asked to begin writing in a daily journal, looking into her past to identify when her problems with pain began.
“I wrote down all the different health symptoms I’ve had throughout my life,” she says, “pain-wise, but also other things” — anything that had caused her distress.
For Jeannine, who grew up in an abusive household, there was a lot of distress, and a lot to write about. (We are not using her last name for reasons of privacy.)
“If I was dressed in a way that my dad thought was too provocative, it wasn’t anything for him to call me a ‘whore,’ ” she says, “and he’d call my mother that too.”
The aggression was also physical, she says. “Lots of pushing, shoving, hitting and certainly a lot of belts in childhood.”
It didn’t take much therapy for Jeannine to discover something that startled her. The backaches, stomachaches, headaches and even skin problems she suffered in childhood tended to occur around the same time as the hitting and the yelling.
It was “just amazing to make that connection,” she says. “I had never really stopped to think about it that way.”
As a young adult, Jeannine moved out of the house. The abuse stopped. But her pain didn’t.
Lumley says researchers are finding that this is the case for a number of patients with medically unexplained pain. He says studies have followed people prospectively over the course of years, trying to predict who develops widespread chronic pain.
“They clearly show that difficult life experiences, adverse experiences in childhood are later predictors of chronic pain — widespread pain — years later,” Lumley says.
Jeannine says the idea that there could be a connection between her pain today and the trauma she suffered during childhood sounded “kind of crazy” initially.
“To me it just doesn’t sound logical,” she says. “You think about pain like something [that] hits you. Something hurts; it’s physical. It’s not like something hits you emotionally and then it hurts.” But in fact, that’s exactly how it can happen, researchers say.
“This is a real phenomenon,” says neuroscientist Amy Arnsten, a professor of neuroscience and psychology at Yale School of Medicine. Under healthy conditions, she says, higher circuits in a part of the brain — the prefrontal cortex — can regulate whether individuals feel pain and how much pain they feel.
But these higher brain circuits can weaken and even atrophy when we’re exposed to chronic stress, Arnsten says, “especially stressors where we feel uncontrolled or frightened.”

(Jessica Pons for NPR)
Fear, depression and anxiety are the sorts of stressors that can weaken these brain circuits, she says, making people more vulnerable to feeling pain. And if those prefrontal circuits aren’t working to help regulate the sensation, Arnsten says, individuals may feel prolonged pain long after a physical injury has healed.
What’s more, without proper regulation, she says, the brain can generate pain when there’s no physical damage. “The brain actually has pathways where it can go down and control our body,” she says, “and actually create a pain response.”
And that pain is very real.
The same thing can happen to adults who suffer trauma, Lumley says. But, when it starts in childhood, that sort of cycle can set in motion a lifetime of chronic pain.
“Most people don’t necessarily outgrow so easily some of those difficult early-childhood experiences,” he says. “Even though one’s life might look good now, people still remain haunted, as memories or thoughts about family come to the fore.”
And that was what was happening to Jeannine at a specific time every day during the week.
“Literally on the drive home, I would start getting pain,” she says.
At first she thought it might have to do with her long commute or maybe how she was sitting. So she got better lumbar support and put “heating elements” in the car’s seat.
But in therapy she realized it wasn’t the car or the commute. It was going home.
“Nothing bad is meeting me here on the drive home,” she says. “But when I was younger, walking home was like, ‘Ahhh, I go back there again?’ It was just a dreadful feeling of ‘Now I have to go back to that environment.’ My house never felt like a safe place for me.”
Fear, she realized, had carried over into her relationships as an adult too, even though she’s now happily married and holds a good management job in a large corporation. She had become deeply hesitant to ever express negative feelings she feared might alienate family, friends or colleagues at work.
“So I decided not to speak honestly. That was my M.O.,” Jeannine says. And that would often be followed by physical pain. In her mind, in such instances, it was easier just to deal with the pain than run the risk of losing the emotional connection with people she cared about.
Today, using the tools of EAET, Jeannine says she has learned how to confront what happened to her as a child and begin the process of healing as an adult. She has learned to be more honest with herself and others about what she really thinks and what she wants.
Lumley says EAET helps some patients look beneath the shame, fear and guilt they may be feeling now to emotions they experienced during the abuse but long suppressed — anger, sadness or distress over the loss of love.

Jessica Pons for NPR)
Patients have to face their fears head-on, Lumley says.
“Part of facing it means talking about it, giving it some expression with your words and your face and your body.”
“The insight and perspective we get from therapy can help us feel more in control,” neuroscientist Arnsten says, “and that can put higher brain circuits back online and allow them to regulate our pain pathways, just as they would in a healthy brain.”
Payne, Jeannine’s therapist, says Jeannine’s journey to health wasn’t easy. “It got very tough and the pain got a lot worse, and it became more persistent.”
But Jeannine persevered and worked with Payne to complete all the written exercises and discussions that were part of the treatment.
Just months after beginning therapy, Jeannine began to engage in conversations she had long avoided — being more honest about her feelings with colleagues and her family. “It was the hardest thing I’ve ever done in my life,” she says.
Now, this is a relatively new therapy, and so far the published evidence of its effectiveness is largely based on one study. More research, with larger studies, is needed to truly gauge its worth.
But Jeannine says the therapy worked for her. Today, she doesn’t avoid situations, people or potential confrontations. She’s relieved. And happy. And her pain, she says, is way down. On some days, she has no pain at all.
9(MDAzMzI1ODY3MDEyMzkzOTE3NjIxNDg3MQ001))