Philadelphia’s 2020 HIV rates mirror reduced screenings over the pandemic
Diagnoses in people who inject drugs were rising before the pandemic. Health officials worry now about spread among people who don’t know their HIV status.
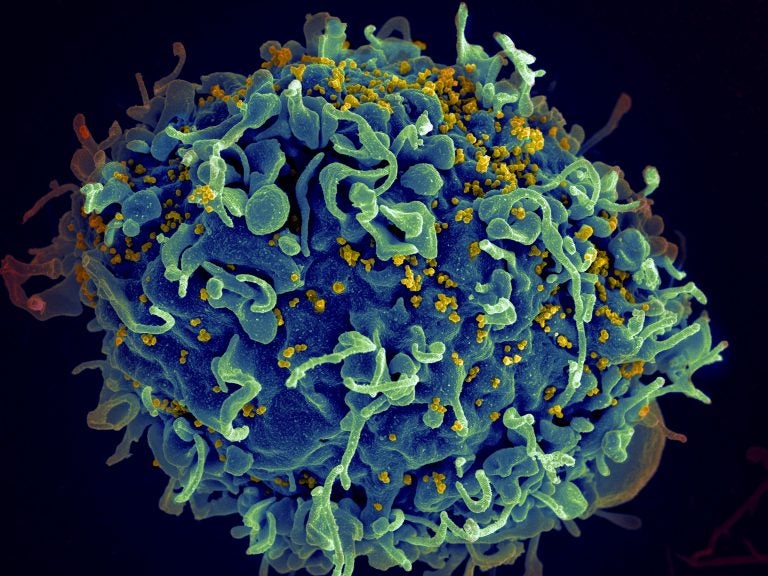
This electron microscope image made available by the U.S. National Institutes of Health shows a human T cell, in blue, under attack by HIV, in yellow, the virus that causes AIDS. (Seth Pincus, Elizabeth Fischer, Austin Athman/National Institute of Allergy and Infectious Diseases/NIH via AP)
The number of reported cases of newly diagnosed HIV infections in Philadelphia declined last year, to 332 in 2020 from 446 in 2019 — but that’s not because the spread of the human immunodeficiency virus is declining.
Health experts say HIV screening has declined significantly in the pandemic, especially during last year’s stay-at-home orders, from almost 7,000 screenings in February 2020 to just over 2,000 in April of that year. Testing levels still haven’t caught up to pre-pandemic times. That means many Philadelphians may be unaware they’re infected, health experts fear.
“We know that the majority of new HIV infections are acquired from people who have HIV but are unaware of their HIV status,” said Dr. Kathleen Brady, acting director of the city’s Department of Public Health. “Our concern is that that proportion, and the size of that population, is now increasing, which certainly is concerning for ongoing HIV transmission and an increase in new HIV infections over time.”
Brady and other health experts are particularly concerned about the spread of HIV among people who inject drugs. HIV continues to affect men who have sex with men, but HIV rates are increasing among people who inject drugs. Overall, both prevalent disease and new diagnoses continue to disproportionally affect communities of color.
As WHYY News reported last month, infections among people who inject drugs have been increasing since 2016. In 2019, 83 Philadelphians who inject drugs were newly diagnosed with HIV, compared to just 33 in 2016.
During 2020, there were only 36 reported new HIV diagnoses among this community, which Brady said was because of the declining access to testing in the pandemic. She added that this population already faces barriers to care, sometimes including limited transportation or phone access, and unstable housing.
“If you don’t test, you can’t diagnose. So it’s very concerning to me that we don’t know what’s happening with that outbreak at this point in time because the places where people who inject drugs typically would get tested are community-based status-neutral HIV testing sites, are frequently emergency departments, and the testing in those sites declined significantly during the pandemic,” Brady said. “I’m very concerned there could be ongoing HIV transmission in that community, and very worried about a further increase in the outbreak.”
The proportion of newly diagnosed HIV cases that included concurrent AIDS diagnoses increased to 17.8% in 2020, compared to 13% in 2019. However, the actual number of concurrent HIV and AIDS cases were about the same over that period. Brady said the data suggests that people diagnosed with AIDS did, indeed, get tested despite the pandemic because they had symptoms. On the other hand, people who felt healthy and didn’t believe they were at risk for HIV did not get tested.
Brady doesn’t expect a sharp spike in documented HIV cases in 2021, because HIV testing hasn’t resumed to normal levels. But the city is launching some new initiatives to increase access to testing. She estimated that once those initiatives are implemented, new HIV diagnoses will rise because of cases that were not captured in the pandemic.
The efforts are part of the Ending the HIV Epidemic: A Plan for America (EHE) initiative, for which Philadelphia and 47 other counties in the United States received federal funding to combat HIV. The goal is a 75% reduction in new HIV diagnoses by 2025 and a 90% reduction in new HIV diagnoses by 2030.
Among the city’s efforts are the opening of four sexual health sites providing wraparound services, such as testing for sexually transmitted infections, pregnancy testing, and referrals to PrEP, a medication that prevents HIV-negative people from becoming positive. The sites are located at Bebashi – Transition to Hope to reach the Black community, Congreso de Latinos Unidos to reach the Latino population, the Mazzoni Center to serve the LGBTQ community, and Courage Medical in Southwest Philadelphia, where there is a lack of access to HIV prevention services.
The sites are modeled after programs in New York City that have demonstrated that people are more likely to get tested for HIV during appointments for other types of screenings.
“We have data that shows that sites like this that we’ve had in Philadelphia are much more likely to diagnose people with HIV compared to stand-alone traditional community-based organizations that do HIV testing,” Brady said.
In 2022, the city will also conduct a behavioral survey funded by the Centers for Disease Control and Prevention that aims to help it to better understand the HIV outbreak among people who inject drugs.
The 30-minute survey will ask people about their sexual and drug-using behaviors, access to prevention services, HIV testing, PrEP, and HIV treatment and care. Brady said that will help the city understand gaps in care, how health officials can intervene to prevent HIV transmission, and help it promote HIV prevention and get funding.
In addition to increased HIV testing, Brady said she would like to see increased immediate linkage to care and access to antiretroviral therapy, increased access to PrEP among people who inject drugs, and increased syringe service programs. In the 10 years after implementation of Philadelphia’s syringe services program, about 10,000 HIV infections were averted, Brady said, noting that these services are particularly important as the use of fentanyl continues to rise. The powerful synthetic opioid has a shorter duration of action than pure heroin, which means people often are injecting 10 to 15 times a day.
“That means they need a clean syringe to use every single time,” Brady said. “That means we need a greater availability of syringe services to people who inject drugs, so that they can use a clean needle every single time that they inject.”

Saturdays just got more interesting.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.