Penn team reports more success with enlisting patient’s cells to fight leukemia
The University of Pennsylvania is reporting more success in its efforts to amp up the body’s own defense system to kill tough-to-treat blood cancer.
Penn’s Abramson Cancer Center garnered national attention when the team helped two men with chronic lymphocytic leukemia become cancer free.
“Now, three years later, they are still in remission, with no evidence of leukemia. So, the response now is durable,” said Dr. Carl June, a director of translational research at Abramson.
“We’ve now treated about 35 men,” June said. “And find that it’s about a 50 percent response rate.”
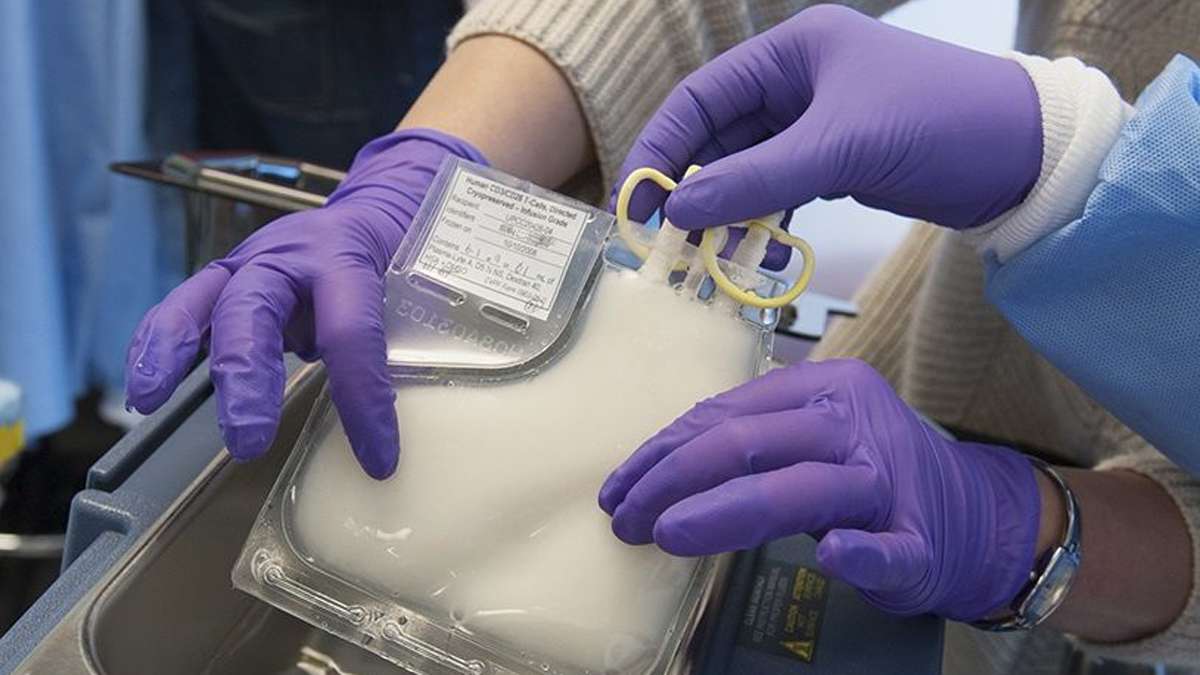
The technique is used only for select patients after a battery of traditional drugs and procedures fails. In the treatment, doctors remove millions of T cells from the patient’s body. They then use a disabled form of HIV to carry new genes into those cells. When the altered T cells are returned to the body, the new genetic material programs them to fight cancer.
In March, Lehigh Valley resident Bob Levis was feeling miserable. He had a temperature of 104, chills and stomach trouble, but Levis and his doctors couldn’t have been happier. His body was weathering something called a “cytokine storm,” which in his case was a good sign that the immune system was fighting hard.
“They actually want you to have a high fever, and get a reaction to these T cells which is evidence that they are becoming a part of my system and are there to fight and kill cancerous leukemic cells,” Levis said.
Levis was among 59 patients — adults and children with two different types of leukemia — who have received the experimental treatment from the Penn team.
“In the past it was: ‘Can we prove that this works and it’s worth that investment?’ Now that’s happened,” June said. “A number of boutique cancer centers have done this and have results similar to what we have.”
Levis is in remission.
“The risk was that it just wouldn’t work,” he said. “I didn’t have many options at that time so I said, ‘Let’s try it.'”
Extending the treatment to more patients
Penn is now looking to make the experimental treatment available to more people, as well as attempting the same technique to treat other kinds of cancer.
“The problem with our current cell therapy is it requires scientists to do this for each patient, and there’s not enough scientists to treat everyone,” June said. “But if we can make it with robots, then it can be done so everyone can have it.”
“Really, it’s not a science issue anymore, it’s an engineering issue,” he said.
About a year ago, the university hospital partnered with drug maker Novartis to do that work.The technique by June and his team is part of an emerging branch of cancer treatment called immunotherapy, designed to rally the power of the body’s immune system.
One benefit of that approach, scientists hope, is that patients won’t have to undergo many rounds of treatment.
Instead, the reprogrammed T cells replicate themselves to provide a kind of “constant source chemotherapy,” remaining “on guard” protect against recurring cancer.
The newly built T cells target tumor cells using an antibody-like protein, called a chimeric antigen receptor.
“It’s still early days, but at this point, one treatment appears to be a sufficient,” June said.
Penn researchers are reporting their results this weekend at a meeting of the American Society of Hematology in New Orleans.
Fifteen of 32 adult patients with chronic lymphocytic leukemia responded to the therapy. Seven experienced a complete remission.
Nineteen of 22 pediatric patients with acute lymphoblastic leukemia experienced complete remissions. Five of the children later relapsed.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.