Games and gadgets: Turning to tech to fight ‘lazy eye’
The goal is simple: saving sight in the amblyopia-affected eye. To keep children from abandoning treatment, researchers are experimenting.

Three children in 100 have amblyopia or “lazy eye,” a vision-robbing, brain-connected disorder that typically affects just one eye. (Brad Larrison for WHYY)
How do we help children thrive and stay healthy in today’s world? Check out our Modern Kids series for more stories.
For those researching amblyopia, also known as “lazy eye,” the goal is simple: to save the sight in a child’s affected eye.
But the shots on goal have varied widely — think specialized video games and 3D eyeglasses; virtual-reality goggles; near-instantaneous diagnostics; and many how-long-do-I-need-to-wear-these-glasses- or patches-studies. All in an effort to keep kids from abandoning treatment.
At Salus University in Elkins Park, optometrist Stanley Hatch wants to see how long kids have to wear glasses. Three in every 100 children have amblyopia.
“We could avoid patching if we had the answer regarding glasses … Maybe it will help with battles with home and day care,” Hatch said.
One study found that only about half of young patients obey doctors’ orders — and it might not be all their fault. In a U.K. study of parents’ attitudes, researchers found the grownups resisted their kids’ amblyopia diagnosis and treatment. Among the reasons: confidence in the test; health beliefs; family and social stigma.
A global study that looked at eye-care services based in schools found that “policy-based support, while also attempting to reduce misconceptions and stigma among children and their parents, is crucial” to improving children’s eyesight.
“Socioeconomic status, prior treatment, degree of amblyopia. It’s hard to match all these things,” said Kammi B. Gunton, an ophthalmologist at Philadelphia’s Wills Eye Hospital, referring to why parents and kids don’t pay attention to treatment.
Researchers have turned to technology. One new design had kids with amblyopia wearing 3D-like glasses while they played a video game, the idea is to get the weakened eye in line with the normal eye. But so far, none of the studies has shown much promise. The young patients were already too old, and they didn’t find the games very interesting — at least to play for a good while, every day, for some time.
One idea: Scan sight of all babies
Or maybe the games just don’t work, said Michael X. Repka of the Wilmer Eye Institute at Johns Hopkins, even though a similar trial involving younger children is still recruiting for the video-game study.
A trial involving 7- to 12-year-olds showed “75% [of the youngsters] completed the trial, and showed 57% adherence,” said Repka, who thought the 57% was “actually pretty good.” But the treatment didn’t show any additional benefit compared with prescription glasses.
“We thought [games] would be a really good thing,” said Irene Gottlob, professor in the Department of Neuroscience, Psychology and Behavior at the University of Leicester in England, who was not involved in this study. “They have to be more interesting, and for different ages.”
Gottlob is recruiting for a study that will involve 460 children in five countries. Because it is easier for kids to wear glasses than eye patches, she wants to establish specific lengths of time for how long a patch needs to be worn, for example, at a specific age, at a specific degree of amblyopia, until the bad eye’s prescription matches the good eye, or if another treatment is needed.
“How much patchwork is necessary is the question,” she said.
A company called Luminopia is in preliminary trials with virtual-reality goggles. Repka, the company’s medical monitor, said the patient views two different images that Luminopia takes from the web, with the weak eye’s image manipulated. The aim is for both eyes to eventually be aligned.
David G. Hunter, ophthalmologist in chief at Boston Children’s Hospital, has a different answer: Scan all children while they are still in diapers.
“We don’t know [of the visual disorder’s existence] until it gets picked up by somebody. But if they don’t get scanned, that is a struggle.”
Wills Eye’s Gunton agreed.
“In the past, we needed to wait until children were older to screen to find amblyopia,” said Gunton, who is also an assistant professor at Thomas Jefferson University. “Now, children don’t have to be verbal … At 9 months or 1 year, [we can] rule out amblyopia.”
Ophthalmologists have known they could do this for a while. A 1996 study found that a baby’s sight can be tested with sophisticated instrumentation. That was important because the instruments are objective, the vision experts interviewed said. Relying on charts filled with figures is not objective, and the charts don’t pick up on farsightedness. The 1996 study found that babies born with farsightedness were 13 times more likely to develop strabismus, a condition in which the eye muscles are not balanced and that can lead to amblyopia
Early intervention is key
Since then, screening devices have been developed. But as Hunter pointed out and various studies attest, these devices look for risk factors: Are eye muscles unaligned? Is the baby’s focus off?
“It is the structure of the eye that is telling you what to look at,” Hunter said.
By looking at just risk factors, “you are still missing kids with strabismus.”
Which is the point of blinq, an instrument that has just hit the market. A handheld device, blinq uses a polarized laser light to scan a portion of the retina called the fovea. (If you can see sharply, your fovea is working.) The device scans both eyes at once, assessing whether they are structurally focused. It picks up where the two are looking. If they are not focused, it detects the problem.
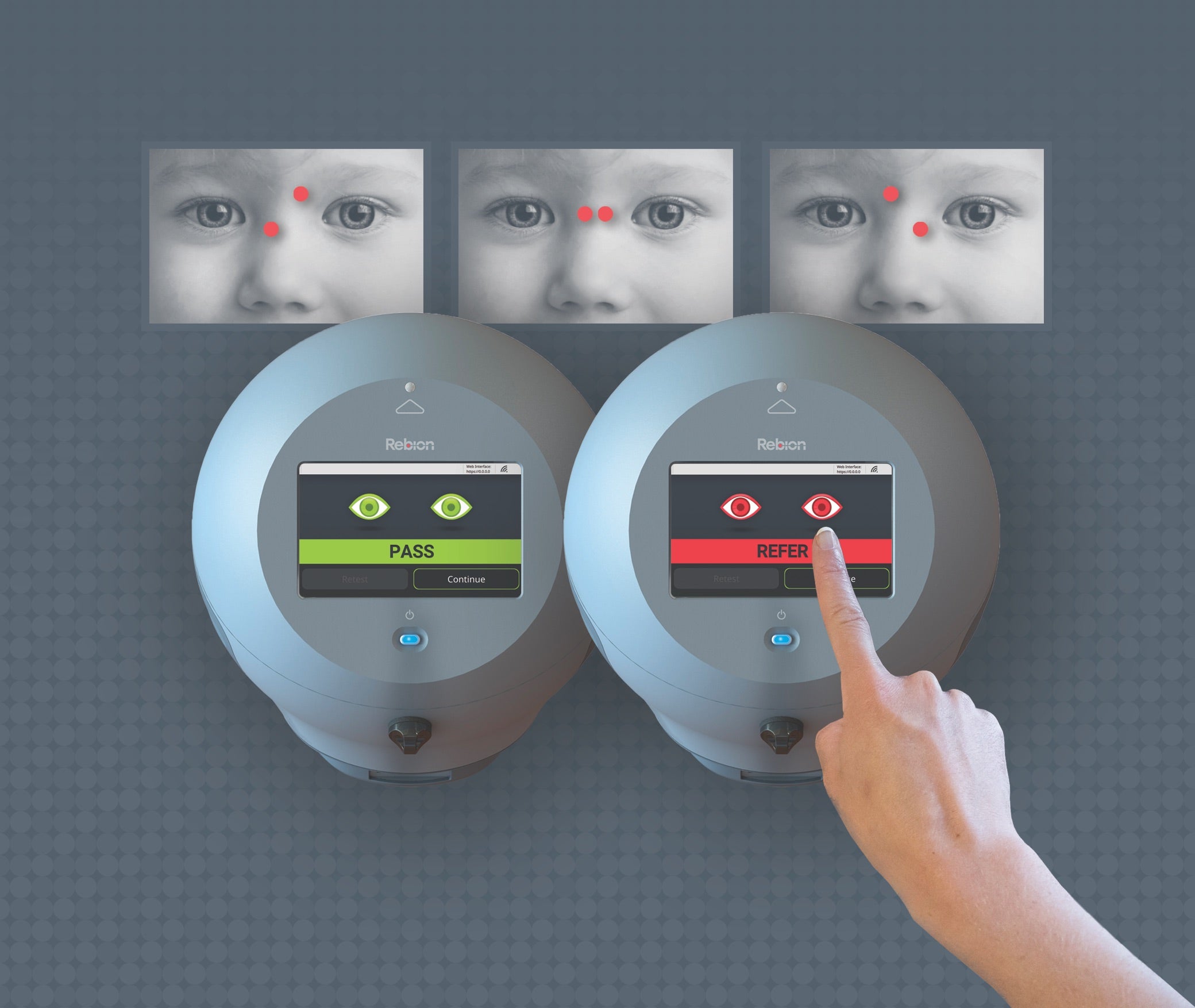
The assessment takes two seconds. A child looks at the smiley face on the small blinq screen and then can hop off mom’s lap.
In an independent study, a prototype of blinq was found to be 97 percent sensitive for strabismus and 94 percent for amblyopia.
Hunter, who worked on the device for about 20 years, said what makes blinq different is that “we can tell who has decreased vision [20/40] so they can’t pass the test … From a public-health perspective, we can focus on kids who need it early on in life.” (If a person has 20/40 vision, he sees at 20 feet what a person with 20/20 vision sees at 40 feet.)
One more point about taking care of children’s vision issues as early as possible:
In a 2018 study of 944 kids ages 4 and 5 years old in Bradford, a large, multi-ethnic city in the U.K., who researchers followed for two years, about half of them had failed a vision test — a percentage that is not considered unusual. Those who wore their glasses the most were also the most literate, regardless of their backgrounds.
The researchers are now preparing another study, looking at what happens when kids who fail vision tests get school-issued glasses and their parents and schools get their screening results. They are recruiting 100 schools to participate in the two-year study.
Parents, the researchers wrote, think support from the schools helps with their “children’s attendance and [sticking to wearing their glasses].”
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.






