In 50 years, heart transplant surgery hasn’t changed significantly
One million people have end-stage heart failure in North America, and only about 2,400 transplants occur each year due to a lack of viable hearts.
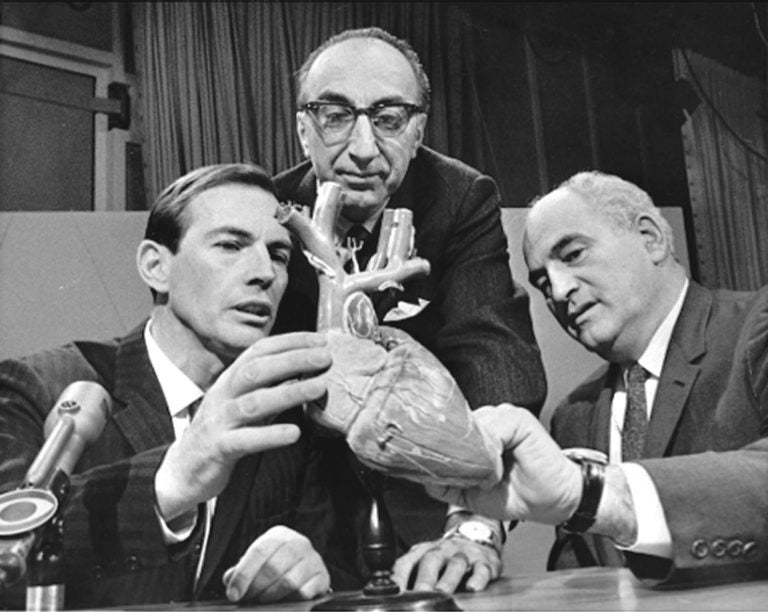
From left, Dr. Christiaan Barnard of South Africa, Dr. Michael DeBakey of Houston and Dr. Adrian Kantrowitz of Brooklyn right, confer Dec. 24, 1967, in Washington, before appearing on "Face the Nation." Barnard performed history's first human heart transplant earlier that month. (AP file photo)
It’s been 50 years since South African Dr. Christiaan Barnard performed the first human heart transplant.
The main difference between that groundbreaking procedure and those performed these days has less to do with the surgery itself — and more to do with the drugs doctors give their patients after the surgery.
“You have to realize that the the body sees the new heart as something that’s foreign. And so the immune system seeks to destroy it,” said Dr. Rhondalyn McLean, medical director of the heart transplant program at the University of Pennsylvania.
As doctors worked more on developing effective drugs to suppress the immune system, the success rate of heart transplants improved. The first heart transplant patient died 18 days after his surgery. Now, most patients live an average of 13 years after receiving a new heart.
But there’s a big problem. McLean estimates around 1 million people have end-stage heart failure in North America, and only about 2,400 heart transplants occur each year because of a lack of viable organs. That number has stayed fairly constant over the years.
However, McLean said, here have been advances in heart-assist devices.
“Maybe about three years ago, the life expectancy of someone who had a heart-assist device would be about 18 months, and now it’s much longer,” she said.
The newer devices provide a survival rate of about four years as a patient waits for an available heart.
Researchers are now focused on how to sustain hearts beyond the four-hour window the organs remain viable once removed from a body.
“If we could you know find a way to increase that window, then you could potentially take a heart from California, and transplant someone in New York,” she says. “Right now we can’t do that, because of the time and the distance.”
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.




