40 years later, scientist who first discovered Legionnaires’ disease is still learning lessons
Listen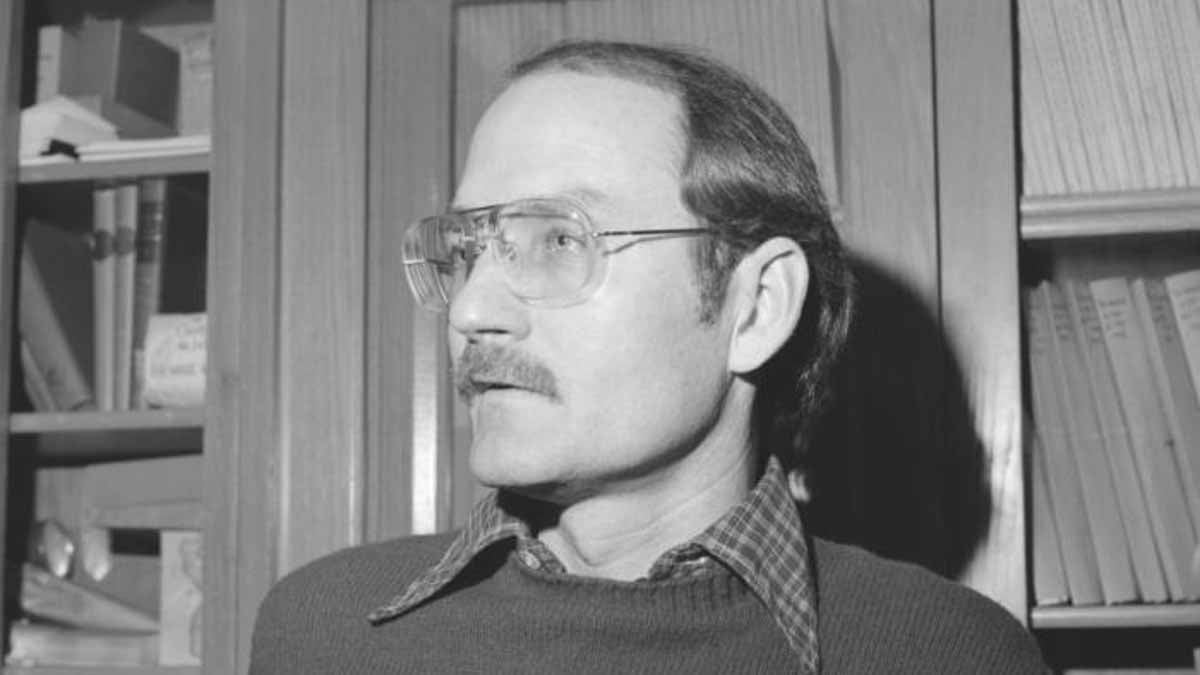
Dr. Joseph McDade is best known for isolating and identifying Legionella pneumophila, the bacterium that causes ‘Legionnaires' disease’. (Public domain image, CDC)
This month marks the 40-year anniversary of the infamous Legionnaires’ disease outbreak in Philadelphia, which, in turn, led to the discovery of the disease itself.
Click here to listen to The Pulse’s audio documentary on the discovery of legionnaires disease in Philadelphia
In July of 1976, just weeks after Philadelphia hosted the nation’s bicentennial celebration, hundreds of American Legion members descended on the city for their annual statewide convention. It centered around the city’s most iconic hotel, the Bellevue Stratford, located near city hall. But within days of the conference, more than 100 attendees had come down with a severe and mysterious pneumonia.
More than two dozen died.
The public feared it was the start of a deadly flu pandemic. Scientists were stumped, spurring the largest CDC field investigation in its history. Congress was frustrated. The hotel shut down.
But it wasn’t until five months later, around Christmas, that a CDC microbiologist named Joseph McDade made a fateful discovery in identifying the legionella bacteria. It would be key to solving the mystery, once and for all.
So how did he do it?
A ‘backbencher’ CDC scientist
“My job at the time of the outbreak investigation was to rule in or rule out whether the disease was rickettsial in origin,” recalled McDade, who is 76 years old now and 36 at the time.
A self described “backbencher,” McDade, who grew up in western Maryland, had recently been hired at the Centers for Disease Control and Prevention in Atlanta. His small unit specialized rickettsial diseases, a type of disease that’s typically transmitted by arthropods like fleas, lice and ticks to other animals and humans. They were tasked with seeing if Q fever had caused the illnesses, which causes a less serious pneumonia.
“It seemed kind of unlikely because there seemed to be no direct contact with any domestic animals in Philadelphia,” he said. “The only other possibility would be contact with dairy products…unpasteurized milk or cheese. And there was no evidence of that.”
But immediately following the outbreak, McDade ran the tests anyway. Nothing came up. Well, at least, it seemed like nothing. He did take a slight note of one seemingly insignificant detail.
“In the course of my work trying to rule out Q fever, I noticed every now and again an occasional rod shaped bacterium in some of the tissues, which was considered to be inconsequential because nobody else saw it,” McDade recalled. “We couldn’t get any bacteria to grow, so at that point in time I just considered it was an extraneous kind of contaminant.”
So, that’s where he and others initially left things: bacteria couldn’t possibly be the source.
“There was nothing that was pointing to it being a bacteria. The pathology was nondescript. They couldn’t see anything, they couldn’t grow anything, nothing looked like bacteria,” said McDade.
Months later, though, a tense social interaction and a yearly ritual would challenge those core assumptions.
“Over time, whenever the various theories for etiology fall away, you sometimes wonder whether or not it had anything to do with it or not, however unlikely,” he said.
And he would soon be reminded to be weary of considering something a scientific fact, in this case, that it couldn’t be a bacteria, no matter how obvious.
“Allow for the possibility that there is something different.”
An awkward Christmas party
In the weeks that followed the July outbreak, pressure mounted on health leaders to figure out what had happened. Congress was publicly grilling top health leaders, accusing them of making mistakes all along the way. And during a time when many thought science had finally beat infectious diseases and largely figured them out, the Legionnaires’ mystery was viewed as a major failure.
“I was way out of the limelight at that particular point in time,” said McDade, who remembers how his behind-the-scenes laboratory role made him mostly “inured” to that stress.
But four months later, around Christmas, McDade did have his unpleasant moment in a spotlight of sorts. It was a moment that would play an important part in McDade’s future discovery and it took place at a holiday party among casual acquaintances.
McDade recalls a man had approached him. They’d never met before.
“I can’t remember his name, I can’t remember what he looks like, but I can remember what he said. He said he was just really disappointed in the CDC. He said, ‘I know some of you scientists are sort of, kind of strange, but we count on you when these sorts of things come up, that you’re able to figure these things out,” McDade said. “He went on for a little while. His tone of his voice was very clear: he was very, very disappointed. I don’t know how much of the festivities [and drinking] contributed to loosening his tongue or not, but anyway, it gave me cause to pause.”
McDade said the interaction motivated him to go back and try harder to figure out what he might have missed.
Another factor was at play, too: McDade’s compulsive nature. As a scientist, he said he’s constantly checking and rechecking his work. The winter break offers an especially good time for this.
“I have a habit, I’ve done this for years, that every year between Christmas and New Years when everything is very quiet…I love to go in [the lab] by myself. Because it’s a chance to go through all your materials, throw away excess stuff, clean out this or that, and tidy up loose ends,” said McDade. “So I thought, ‘you know what I need to do? Is go back and take one last look at the impression smears, the slides of guinea pig tissue that I looked at before, to make sure I didn’t miss anything.”
McDade is referring to the slides of samples from guinea pigs that had initially been injected with tissue from the lungs of people who’d died from the mysterious illness. It’s an approach scientists often use to try and isolate a potential organism that has been infecting people. Scientists screened these guinea pig samples for dozens of viruses, bacteria and other infectious agents.
So McDade went back to the lab that quiet holiday week to review the guinea pig tissue that was used during the initial testing to rule out different sources of the Legionnaires’ outbreak.
In a newspaper interview at the time, he had likened the process of zeroing in on that tissue under the microscope to searching for a missing contact lens on a basketball court with your eyes four inches away from the floor.
‘Apple green fluorescence’
“I sat there, and I looked at [the slides] for a very long period of time, and I didn’t see much,” said McDade.
The only thing he did see was an occasional rod shaped organism, the one that was so rare that he and others had discounted it before.
“And all of a sudden, I came across one microscopic field that appeared to have a cluster of microscopic [rod-shaped] organisms. Not just one, but a cluster,” Mcdade recalled. “Maybe a half a dozen to a dozen, which suggested to me that they were replicating there at that particular site.”
McDade still didn’t think it was meaningful, but being the compulsive type, he decided to run the tests again and see if he could grow those rods through new lab cultures.
“And if I can’t, then I can show once and for all it has nothing to do with the outbreak. And then I can stop thinking about this,” he said. “Or if it turns out to be something, so be it.”
It was something.
McDade’s lab reran the tests, with a few modifications that he thought would ensure whatever might be present and causing this disease could grow. The actual culturing and testing process is very complex, but it basically involves taking tissue from those guinea pigs, which had been injected with material from the people who’d been sickened with legionnaires disease, and then injecting that into the egg yolks of hens (Previously, McDade had added an antibiotic mixture to prevent the growth of bacteria while he isolated the possible presence of Q fever, which was his lab’s main directive. This second time, he didn’t add the mixture, enabling any potentially contaminating bacteria to grow).
When infected eggs didn’t do well and died, McDade then examined samples through a special preparation and staining process.
What he saw under the microscope struck him: lots and lots of rods radiating a “brilliant apple green fluorescence,” a result of the chemical staining process.
“I could see [the samples] were just absolutely full of bacteria,” said McDade.
Mcdade said he was still cautious at this point. He still wasn’t sure whether the bacteria had come from the outbreak or somewhere else, whether it was a cause of the mysterious illness or just an association.
His lab then did additional testing to see if the blood samples saved from people who had died of Legionnaires’ disease contained antibodies to this bacteria that weren’t present in blood samples from earlier stages of their illness. If the bacteria had been the cause, their blood would contain lots of antibodies for the bacteria after they’d gotten really sick (antibodies are special proteins that the body’s immune system develops in an attempt to identify and fight off foreign substances).
Tests then confirmed the bacteria was present in those who had become really sick and died, further pointing to it being the cause.
“I can tell you the moment, that it was was very late one evening, and there were two or three of us, it was that small of a group, we were clustered back in a little closeted area looking at the results,” recalled McDade. “And as we broke the code and found out that they were falling into this particular pattern, I can still remember the hair raising up on the back of my neck because you knew this was highly suspicious and highly suspect, and it certainly gives you – I won’t say it’s a charge – but it certainly does get your attention whenever something like that happens.
It was a pivotal moment.
McDade had identified the agent that had caused the mysterious pneumonia at the Legionnaires’ convention. It was a bacteria that scientists had never been seen before. They called it legionella.
Additional studies would further confirm the bacteria as the cause. The health investigation went from being viewed as a total flop to a success.
A chance discovery?
In the public health world, Legionnaires’ disease is often viewed as a classic case of the power of epidemiology, and its core tools that field investigators use to map out patterns and understand how diseases strike.
But what if McDade never went back to the lab that Christmas and meticulously reviewed his samples? Did the whole success of the Philadelphia legionnaires’ mystery come down to a chance discovery by a scientist who voluntarily decided to take a second look, following an uncomfortable encounter at a holiday party?
McDade says no, not entirely.
“There are a lot of people who think chance plays a large part in the discovery, and I suppose it does. But I think the methodology brings it all around eventually,” he said. “I think that one of the things that happens over time is that scientists peruse the same areas, and sometimes they go back and try to reproduce what other people do, and reinvestigate it. And things then come out.”
In the case of the Legionnaires’ disease discovery, Mcdade said the disease itself wasn’t new. But without a big, fatal outbreak, sporadic cases often went unnoticed.
“However when you get a very large outbreak of something, with 150 to 200 cases of disease, it cannot be ignored. It cannot be ignored,” said McDade. “Sometimes what it takes is a large outbreak of a disease to help you discover something that’s been percolating for a long time, undetected.”
Following the discovery of the legionella bacteria, he and others were then able to trace it back to previous, unsolved outbreaks.
“I still to this day continue to learn lessons,” said McDade. “Data becomes information, information becomes knowledge and hopefully someday knowledge collectively becomes wisdom.”
Applying the lessons of Legionnaires’ to a career in public health
Mcdade could have turned his life’s work into studying Legionnaires’ disease, but he didn’t.
And while he admits that many would consider his identifying the legionella bacteria as the biggest discovery of his career, he said he used what he learned from that experience to make “equally satisfying” contributions to public health throughout his life.
One of McDade’s biggest lessons from working on Philadelphia’s Legionnaires’ outbreak was the way it transformed his entire scientific approach. Up until then, he focused on making sure he ran tests well and accurately.
“I was trained as a research microbiologist and not as a public health microbiologist,” said McDade. “And the more I learned about epidemiology, the better a laboratory scientist I became. Because it’s not only about doing the right tests and doing them well, it’s knowing what to test and why. And I found that over time, I started asking the broader questions about what do we think is happening, how can we determine what that is, what tests we should perform and why,” said McDade. “If you’re not asking the right questions about it, the information won’t necessarily be useful.”
He began collaborating more with people.
After three years of working on the outbreak, he went back to the rickettsia field, where in the mid-1980s, he helped discover the first human case of ehrlichiosis, a disease which up until then, was thought to be confined to dogs. McDade recalled drawing parallels between the then mysterious human case that others thought could be rocky mountain spotted fever and an image he had seen during a military presentation years earlier of a terrible Ehrlichia infection that army dogs had contracted from ticks.
Mcdade later became deputy director of the CDC’s national infectious disease center. Pointing to the lessons from Legionnaires’ of the importance of collective knowledge and collaboration, he launched one of the first online open access journals, Emerging Infectious Diseases, in the 90s and was editor for five years.
“The idea was to improve communication around the world about emerging threats, and it worked very, very well and rapidly,” he said.
The popular journal is now monthly. McDade also taught at Berry College in Rome, Georgia. He retired in 2014 and is now a member of the National Institute of Health’s national science advisory board for biosecurity.
“That’s my only professional activity at this point. Otherwise, I find myself very busy every day. A lot of it is fun, some of it is a bit of work, but I don’t sit still well,” said Mcdade, laughing.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.

