On the move: Mobile health teams are taking medicine to the street in Philly
Street medicine teams that provide care for people who are unhoused hope that new Medicaid reimbursements will help them expand operations.
Listen 5:49
File: In this Feb. 19, 2016, photo, a physician assistant checks a vacant homeless camp in an attempt to provide medical care. (AP Photo/Matt Slocum)
From Philly and the Pa. suburbs to South Jersey and Delaware, what would you like WHYY News to cover? Let us know!
From the passenger seat of an SUV headed down a local street in North Philadelphia, nurse practitioner Kara Cohen leaned out the window and yelled out to a man walking by on the sidewalk.
“You! Buddy!”
Sam Santiago, who was driving, twisted the wheel to the right and brought the car to a sudden stop at the curb, and Cohen jumped out.
“I heard you’re back at the place,” she told the man — her patient — as she pulled out her medic bag and set up a collapsible stool on the sidewalk. “I was so happy.”
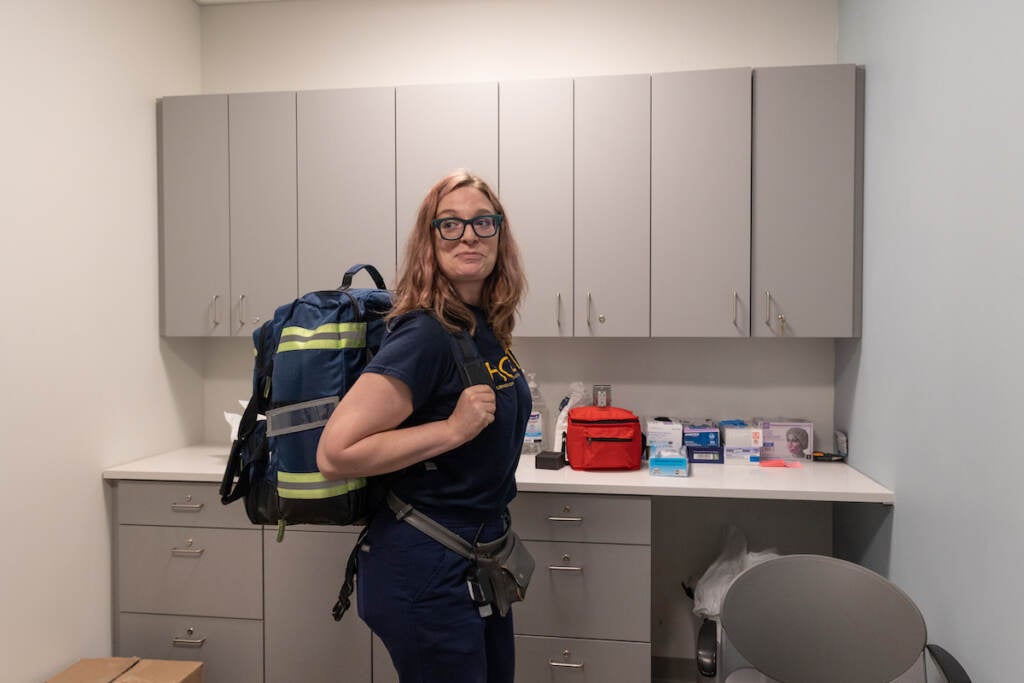
Cohen is the medical director of Project HOME’s street medicine program. This team of health and outreach workers spends a lot of time driving around the neighborhood of Kensington to meet people on sidewalks, street corners, in parking lots, and under bridges.

This is where they provide medical care and treatment for injuries, illnesses, and chronic diseases to patients who are homeless and who may have complex needs like mental health issues or substance use disorders.
Until recently, health workers practicing street medicine haven’t been able to bill or collect reimbursement for their services from insurance providers when providing care outside the four walls of a clinic, hospital, or office.
But expanded insurance coverage and service code changes this year in Pennsylvania and at the federal level now recognize street locations as legitimate environments where health care services are delivered.
It means providers can now get paid for their work through programs like Medicaid. They hope it will strengthen and better sustain programs for them to expand and meet a growing demand in homelessness services.
“It can be a way to make it viable for excellent care to be provided,” Cohen said. “I’m hoping the kind of care that comes out, like when teams are being made, are things that are held to the same standards as we would expect from brick-and-mortar places, that there’s documentation, consent, abiding by medical ethics, that there’s an attempt for dignity and consistency.”
Intensive work and potential barriers to reimbursement
As she sat next to the car and used the open passenger door as a makeshift privacy curtain, Cohen unwrapped some gauze on her patient’s hand to check on a healing wound.
“I’m going to just put some maybe A+D [ointment] on it and clean it up,” she told the man, who she’s been seeing for a couple months now.
Cohen asked if she could find him tomorrow to take some blood work, and listened as he talked about potentially enrolling in medication-assisted treatment for substance use.
It can be difficult for people who are homeless to access medical care in general, Cohen said, with many of her patients feeling unwelcome and judged at private health offices because of their housing circumstances.
It can be especially challenging to navigate the health system and appointment schedules for people living with serious mental health issues and addiction, Cohen said.
“Some of our folks, it is so bad that they really are not going to go up the block independently,” she said. “Sometimes, you have to find someone on a corner and bring them to the place where they need to get seen, or do the care right there.”
Wounds are a common issue for people living on the street, particularly for those suffering skin sores and lesions after using drugs containing xylazine, or “tranq.”
In Kensington, there are dedicated wound care units, which is why Cohen and her team try to focus on primary care, where she said there’s a big gap in services for people who are homeless. It’s intensive work, she said.
“We’re managing HIV, Hepatitis C, syphilis, necrotic ulcers, diabetes, hypertension, and asthma,” Cohen said. “All these kinds of things, like pneumonia, acute issues, non-acute issues, and doing it in a trauma informed way.”
Recognizing some long-term health benefits and cost savings, Pennsylvania moved to include street care delivery under its Medicaid coverage this past July.
In October, the Centers for Medicare and Medicaid Services officially added outreach sites and streets to its list of “Place of Service Codes for Professional Claims,” which already includes sites like homeless shelters, schools, offices, private homes, and mobile units.
The updates are welcome news for the street medicine program at Penn Medicine Lancaster General Health, said Dr. Jeffrey Martin, chair of the Department of Family and Community Medicine.
The program is operated by rotating medical residents and has mostly relied on health system funding, grants, and private donations. It will soon expand and hire full-time staff, so Martin hoped the new reimbursements will help in those efforts.
“There’s going to be a lot more visits,” he said. “It’s going to be more coordinated with the rest of the health system and hopefully be able to serve more people.”
But in order to actually bill and get reimbursed for services, Martin said health workers will need to enroll patients in insurance programs like Medicaid, which could be a potential barrier.
“That first goal is going to be establishing relationships and letting them know that, ‘Hey, this is a group of people that are going to be coming out on a regular basis and we care about your health care,’” he said. “At some point as that trust is better developed, they may feel more comfortable giving their information in order to enroll in Medicaid.”
There are also limits on which health providers will be able to bill for services. While Pennsylvania lists doctors, certified nurse midwives, advanced practice clinicians, psychologists, and other professionals as eligible, registered nurses are not individually included.
Julie Dees said she hopes that will eventually change. She is the chief executive officer of the Family Service Association of Bucks County, where a street medicine program is staffed by registered nurses and social workers.
“We’re doing the same work as the ones that do have a physician and we’re having the same outcomes,” Dees said, “so that’s really my frustration with it. I’m excited, because it’s a step in the right direction, but there’s a whole lot to do to improve it.”

‘On the front lines’
Back in the Philadelphia neighborhood of Kensington, Kara Cohen and Sam Santiago continued to drive around as they looked for the familiar faces of their patients.
Along the way, they passed by a young woman who was slumped over against a building, her face bloated and complexion gray.
“Are you OK?” Santiago yelled out the car window. The woman signaled she may need an ambulance.
“Let me pop out,” Cohen said as the car came to a stop.
After quickly checking the woman’s breathing and heart rate, Cohen called for an ambulance, which arrived about 15 minutes later to take the woman to a nearby hospital.
Cohen suspected the woman might have a cardiac problem, possibly heart failure. She texted a friend who works in the emergency room at the nearby hospital to give them a heads up about her new patient, and hoped that she would get an update later.
“It’s just absolutely heart-wrenching to see some folks that are just really trying to survive,” Cohen said. “Sometimes, I kind of feel like we’re working in battle and we’re on the front lines in a war. I go home and it sits with me, and I think about all of our folks and it’s hard. It’s really hard.”
The new service codes and insurance reimbursements should help ease some of the burden, she said, at least financially.
As for the emotional and psychological toll, Cohen said the small individual wins help. They remind her that there’s still opportunities ahead for street medicine to grow and help even more people.

Get daily updates from WHYY News!
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.






