Hundreds of Pa. senior-living facilities haven’t received vaccine as widened eligibility, low supply slow rollout
An analysis shows that more than 300 senior care homes did not have a scheduled vaccine clinic as of Jan. 17, while hundreds more weren’t covered by a federal partnership.
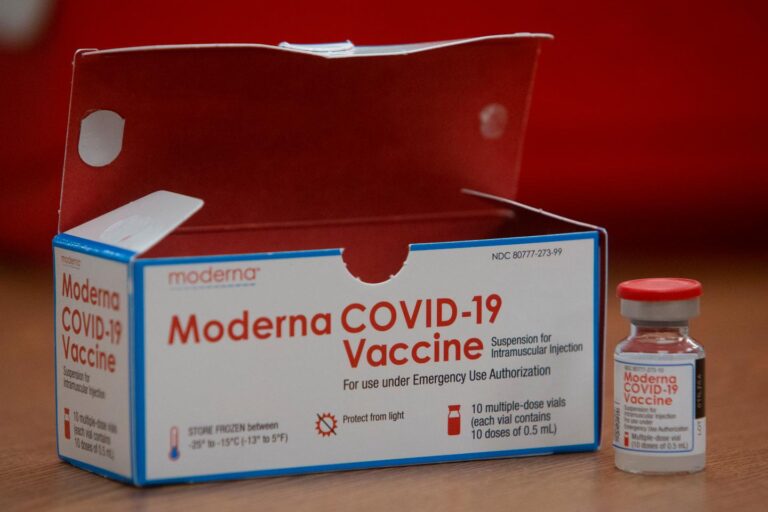
(Alejandro A. Alvarez/Philadelphia Inquirer)
Spotlight PA is an independent, non-partisan newsroom powered by The Philadelphia Inquirer in partnership with PennLive/The Patriot-News, TribLIVE/Pittsburgh Tribune-Review, and WITF Public Media. Sign up for our free newsletters.
After a sluggish start, the vast majority of nursing homes in Pennsylvania have hosted at least one COVID-19 vaccine clinic for residents and staff.
But as Pennsylvania continues to expand who is eligible for a coveted dose during the initial rollout, the same can’t be said of personal care homes and assisted living facilities, where thousands of people have died of the coronavirus.
A Spotlight PA analysis shows that more than 300 long-term care facilities enrolled in a federal vaccination program did not have a scheduled clinic as of the week of Jan. 17. That’s according to data provided by CVS and Walgreens to the state health department, a reporting process that can lag by up to 72 hours.
Those pharmacy chains are responsible for vaccinating thousands of vulnerable seniors in partnership with the Centers for Disease Control and Prevention.
Hundreds of other personal care homes and assisted living facilities, meanwhile, aren’t in the federal program. State agencies have developed a separate effort to vaccinate these residents and staff, but it won’t launch until Wednesday.
The ongoing delays happen as Pennsylvania grapples with a surge in demand after the state once again expanded eligibility for the initial vaccine rollout. Adults 65 and over, and those aged 16 to 64 with some high-risk conditions, were made eligible for the COVID-19 vaccine in mid-January in response to shifting federal guidance.
Gov. Tom Wolf said Tuesday that the state expected the federal government to provide more vaccine supply simultaneously as officials expanded eligibility.
“Well, that was wrong,” he said during an afternoon news conference. “They weren’t expanded. In fact, it turned out that there was no backup stockpile that was going to be thrown open to the market. So it’s been frustrating.”
Through Operation Warp Speed, the federal government allocates a set number of doses to each state. States then get to decide how much of that allotment will go to various priorities, including nursing homes and long-term care facilities.
The Department of Health set aside 39,000 doses “each week for four weeks to ensure we were vaccinating skilled nursing facilities to start,” a spokesperson said. The state is now allocating 45,825 doses weekly “to serve the other long-term care facilities.”
This week, that accounts for 32% of the doses the state distributed. The spokesperson did not explain how the state selected that percentage.
States were also in charge of deciding when CVS and Walgreens could begin scheduling clinics. Officials in Pennsylvania picked late December for nursing homes, where more than 7,000 people have died since the beginning of the pandemic. That lagged other states by one or two weeks, data from the pharmacies shows.
CVS was assigned to 510 of these facilities, while Walgreens is handling another 94. Between them, the pharmacies have administered more than 131,000 doses to residents and staff. Exactly who those doses went to is unclear. CVS and Walgreens do not publicly provide that information, and a health department spokesperson said the agency did not have a breakdown.
Many — but not all — personal care homes and assisted living facilities licensed by the state are also being served by the CVS and Walgreens partnership. But unlike more than two dozen other states, Pennsylvania did not ask the federal program to begin vaccinating people in these facilities until mid-January.
The state health department did not respond to a question about the timing of the decision.
“We seem to be extremely far behind other states in rolling out vaccinations in these settings, and we fear this already devastatingly slow process will only get worse,” said Adam Marles, president and CEO of LeadingAge PA, an association of long-term care providers.
Further complicating the process, a few hundred personal care homes and assisted living facilities didn’t sign up for the federal program in time and weren’t eligible as a result. The state Department of Human Services in mid-January announced it had partnered with pharmacy chain Rite Aid to fill that gap.
“It really did come together really quickly,” said Dr. Doug Jacobs, the department’s chief innovation officer, who is overseeing the Rite Aid partnership. “It took a long time, frankly, for us to verify that the CDC was not able to get additional facilities into the federal pharmacy partnership program, and so as soon as we heard that information we really tried to think critically about what we could do to get our facilities vaccinated.”
Roughly 6,000 facilities qualify for the program, but only about 2,200 have thus far indicated that they would like to participate, a spokesperson for the agency said. About 60 facilities “have scheduled or were contacted to schedule their first vaccine clinic this week.”
While advocates for nursing and personal care homes initially praised the federal pharmacy partnership for helping to standardize the vaccine rollout, the program’s speed has drawn criticism.
Delays were already emerging by early January. Lobbyists said they learned of at least one Pennsylvania home not scheduled to have its first vaccine clinic until March 11. State officials now say they expect the vaccination effort in long-term care facilities to be completed by the end of February.
“We’ve had multiple conversations with both the Department of Health and the governor’s office about this,” Marles said. “Some of it may be on the pharmacy partner side, CVS and Walgreens, some of it may be on the allocation side. It’s been very hard to tie them down to a particular issue, but it’s a tragic situation.”
Pennsylvania is not the only state that has had problems with its vaccine rollout, as the federal government has failed to deliver promised allocations and given states little time to plan. Still, the commonwealth has only administered roughly half of the 1.5 million doses it has been allocated, falling below dozens of other states.
“Pennsylvania is in the middle of the pack,” Wolf said of the state’s “efficiency” getting people vaccinated. “So we recognize that we need to do a better job. I hate being in the middle of anything. I want to be at the top of the pack, and we’re going to continue to work together.”
West Virginia is the only state that opted out of the CVS and Walgreens partnership, relying instead on smaller, local pharmacies — and getting a half-month head start on vaccinating willing long-term care residents, NPR reported. By controlling its supply of vaccines directly, officials there said they were able to move more efficiently and adapt more quickly.
Some local independent pharmacists, who already work with long-term care facilities, were disappointed to not have been tapped to deliver vaccines, said Victoria Elliott, CEO of the Pennsylvania Pharmacists Association.
“And they’ve again been locked out, and they haven’t been the go-to group to help the state get this done, much like they did in West Virginia,” she said.
Zach Shamberg, president and CEO of the Pennsylvania Health Care Association, an industry group, said the state should consider partnering with smaller pharmacies.
“At the end of the day, we’ll work with whoever can get us the vaccine quicker,” he said.

WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.




![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)



