In Philadelphia, profiling life after overdose and Narcan
Listen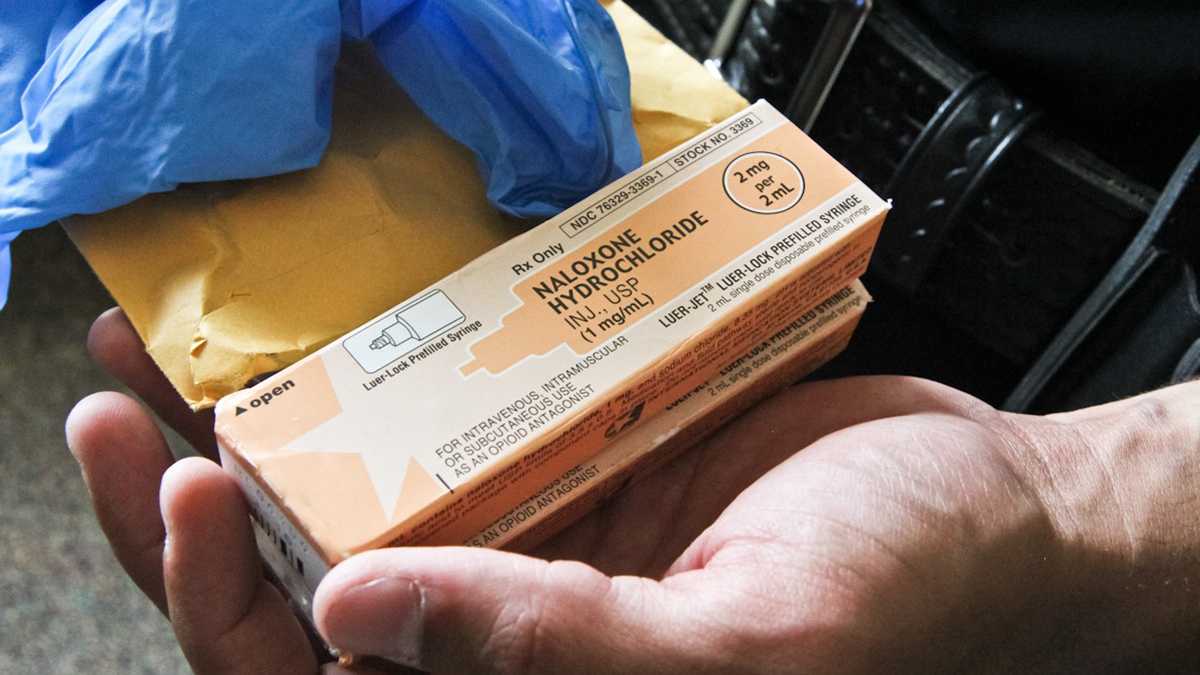
With heroin and prescription painkiller use nearly doubling in the last two decades
Holly Platts could have easily joined the more than 25,000 people annually who die from an opioid-related overdose in the U.S., which, combined with other types of drug overdoses, is the leading cause of accidental death.
It was a hot day in June. Platts was homeless, dehydrated and spent. Looking to get high fast and on the cheap, she recalls taking a hit from an especially potent batch of heroin along a common outdoor drug corridor in north Philadelphia.
The next thing she remembered was waking up in the emergency room.
“I felt horrible, like worse than I had ever felt in my life,” said Platts. “My body had ached, I was shivering, I was cold, I was sweating, I was crying. I didn’t know how to feel. I didn’t know how to act, and I felt desperate.”
Platts, who’s 28 and a mother of two, had never overdosed before, but she immediately knew what happened: naloxone had saved her.
“It takes the opiates right out of your system, so of course you’re very sick,” she said, then adding that “the first thing that popped in my head was, ‘Wow. I can’t believe I almost lost my life.'”

Holly Platts standing in front of the church she regularly attends. On her hip, she has her Narcotics Anonymous badges that symbolize the time she has spent sober. (Paige Pfleger/WHYY)
A life-saving intervention
Naloxone’s power comes from its ability to seep into the receptors of one’s brain and block the opiates, which are causing that depressed heart rate and breathing, from getting in. So if administered soon enough, it can reverse, on the spot, a potentially fatal overdose.
With heroin and prescription painkiller use nearly doubling in the last two decades, naloxone has turned into one of the most powerful weapons against a growing overdose epidemic. While cost and accessibility are ongoing issues, the overdose ‘antidote’ is becoming more widely distributed across the country, to everyone from first responders to those directly at risk of overdosing. Three months ago, Pennsylvania’s physician general issued a standing order – an open prescription – allowing anyone to get naloxone from a pharmacy.
Proponents stress that if available at the right place and the right time, the immediate impact is stunning: a survey of organizations that provide naloxone to community members reported more than 25,000 overdose reversals between 1996 and 2014.
Two years ago, New Jersey put naloxone in the hands of law enforcement, stressing that those minutes, even seconds, it takes to respond to someone who has overdosed could mean the difference between life and death. Last year, the state experienced its first decline in drug overdose deaths in four years.
But then what?
Despite its growing use, what happens, literally, in the moments after Narcan revives someone, paints a much more complex reality of drug use, overdose prevention and health care.
For one, while naloxone is extremely effective, it can be abrupt. Depending on a person’s history of drug use, the type and amount of drugs in his or her system, and the way that naloxone is administered – via spray or injection – a person could suddenly wake up feeling in withdrawal: sick, confused, agitated, even angry.
Many first responders see people walk away after being revived, even though the protocol is to take them to the hospital and encourage follow-up care. Unless that person poses a direct threat to themselves or others, there’s typically not much else they would or could do. In Philadelphia last year, the fire department recorded that 164 people, out of the 3,035 first responders revived with Narcan, declined follow-up and being transferred to a hospital. This doesn’t include community-administered Narcan situations where people may have not have called EMS.(A couple studies have found that administering naloxone alone, without follow-up, is still a very safe intervention.)
Addiction is complicated, and several factors can play into this occurrence. That includes people’s level of drug use and their trust and experiences with law enforcement and the health system, experts say. But for many, like Holly Platts, coming face-to-face with death can be a moment of reckoning.
“You’re contemplating with yourself,” said Platts of that moment after she overdosed last June. “Do you want to go back out and do more, or do you want to not be like this anymore?”
In her case, paramedics did take her to the ER for observation, making her one of the 2,871 people whom Philadelphia responders revived with Narcan and then transported to a hospital in 2015, according to fire department numbers. Typically once there, a person is under watch for about an hour and a half. Narcan blocks any sort of high for at least 30 minutes and then wears off over the subsequent hour. There’s a small risk an overdose could come back, especially if a person overdoses on a long-acting pill.
Platts recalls, in that haze of nearly dying, she wanted help. She asked for it and was kept overnight. She felt drained, like she couldn’t move. But the next day, for a host of factors that included her insurance situation, she says there wasn’t anywhere to go.
No plan.
“So when I left the hospital, the only thing I could think of to feel better was to go get high,” she said. “I just couldn’t take the pain anymore, the suffering. I wouldn’t wish that on anyone. It’s horrible.”
Over the next few months, Platts says she overdosed several more times. Each of those times, naloxone brought her back.
“My intent was never to hurt myself or ultimately die, but unfortunately I came very close quite a few times,” said Platts. “Being that deep in addiction, your mind is clouded, and all I could think is I just wanted to feel better at the time.”
In general, people who overdose are at higher risk for overdosing again. A review of people coming into the emergency room at Boston Medical Center found that on average, a person overdoses about two times.
Platts says after that first overdose, she mostly stopped asking for help in those moments after being revived, even though she thought about it.
A patchwork response
“I do wonder, and I’m frustrated by the situation,” said Dr. Priya Mammen, a professor of emergency medicine at Thomas Jefferson University Hospital in Philadelphia.
Mammen, who used to work at Temple University, is involved in several area groups focused on drug use, overdose responses and prescribing guidelines. She says hospitals typically don’t track what happens to people after a non fatal overdose. Jefferson wasn’t where Platts says she’s was taken to, but even so, Mammen is not surprised by what happened to her.
“To get somebody into treatment or to even to make the linkage is amazingly complex,” Mammen said. “It’s very, very different than someone with diabetes or someone who has these very clear medical issues.”
Community trainings stress the importance of staying with someone who’s just been revived with Narcan and calling for help. Emergency room staff will watch people for a few hours and monitor vital signs, but beyond that, the immediate plans for those who survive an overdose are unclear.
Psychiatric crisis centers, Mammen says, are better equipped for this. Social workers in the hospital can play an important role, but she’s found it’s generally beyond the ER’s scope to make the needed connections.
“Often I’ve reversed someone and I’ve done my best to impress how serious the event was,” she said, adding that other than that, “we have a packet of information of detox and rehab centers around the city, which I find just so unpowerful, to be like ‘Here you go. Here’s a set of papers. I hope you read them. I hope you choose one. I hope you go and call them.”
Even if someone does call for help, she knows a lot of places simply won’t have room.
Post overdose interventions being tested
Public health experts cannot stress enough the benefits of naloxone.
Traci Green, a professor at Brown Medical School in Rhode Island and deputy director of Boston Medical Center’s injury prevention center, is one of them. She says the expanded use of naloxone, in combination with policies that legally protect people in overdose situations, has increased 911 calls in her area and those seeking immediate help.
Which is why, she says, more and more places are starting to focus more intently on that next step, the what happens right after someone gets hit with naloxone.
“I think what we’re seeing is a real rebirth of what can we think about, what can we use in what we understand about how to treat addiction better with this opportunity,” she said.
In most places, including Philadelphia, non fatal overdoses are not reportable, so there isn’t much overall tracking of what happens following an overdose. Rhode Island recently changed that, and is just beginning to collect data. The state is also testing out an idea, says Green, that came out of the recovery community: on-call recovery specialists who essentially respond, within minutes to an emergency department overdose. They offer resources, they follow up, and unlike general medical staff, they also offer a shared experience. It’s a peer-to-peer model.
New Jersey just launched a similar approach in Ocean and Monmouth counties this past month, through a specific state funded pilot, highlighted in New Jersey Governor Chris Christie’s recent state of state address.
“You need somebody who is actually skilled in this area, and the recovery coaches are people who’ve actually walked the walk,” said Joseph Coronato, the prosecutor for Ocean County, the first place in the state to have police carry naloxone and a participant in the new project. “They’re individuals who’ve had a substance abuse problem who’ve overcome that problem and are now working with other people.”
Responses in other states like Massachusetts have involved everything from better training medical staff to having a social worker or first responder who initially saved someone follow up with that person that same day. A program in Connecticut is experimenting with starting people on buprenorphine, often preferred to methadone, right out of the ER. Forced ER observation or treatment has been thrown out there on the other extreme.
Pennsylvania’s department of drug and alcohol programs recently called on county groups that oversee local addiction and treatment efforts to come up with ‘warm hand off’ policies by the end of February for individuals who’ve survived an overdose. No additional funding is attached, but spokesperson Jason Snyder explained via email:
In order to ensure expedient, appropriate and seamless care for an individual who has overdosed, SCAs must develop, implement, and maintain a plan for screening, assessment, treatment and tracking of individuals who have survived a recent overdose. The policy and procedure must include:
1. The details or process by which an overdose survivor will be offered a 24/7 direct referral from the ED to treatment;2. The parties responsible;3. The timelines for the processes involved; and4. The mechanism for tracking such referrals or refusals for treatment.
In general, Philadelphia does not track post non-fatal overdoses, though the Department of Behavioral Health and Addiction Services is looking to start limited tracking in emergency departments.
If all else fails…a DIY approach?
Then there are people like Carol Rostucher, who aren’t waiting for formal programs to roll out. Rostucher carries naloxone in her purse, and spends most of her time driving around a maroon ’98 Toyota Corolla, crisscrossing throughout Philadelphia, connecting and following up with people who are homeless, in active addiction, in and out of treatment, and the ER.

Carol Rostucher drives in her car, with supplies in the back seat. (Elana Gordon/WHYY)
She’s an informal navigator of sorts, “just meeting people where they’re at”, she says, though she also has received addiction training.
On a recent Friday, she picks a guy up from a state funded 90 day recovery house and helps him move to one where he’ll be paying and starting to work.
Her phone rings constantly. She then stops to pass out food, hand-warmers (and hugs) to some others who are homeless.
She takes another person to a methadone clinic, then to a city office to pick up a much-needed transit pass. In the interim, that same person helps Rostucher pass out food in the very spots where just a few weeks earlier, he was out asking for money.
Rostucher used to be a legal assistant, but this has turned into her full-time gig. She has a personal stake in this. Naloxone saved her own kid’s life.
“My son was out in the streets in active addiction, and going to find him, I would see other lost souls,” she said. “And I just felt so horrible. People would drive by and ignore their existence, and I just couldn’t do it.”
In late afternoon, she picks up Salvatorie Mauro. She hands him a bag of toiletries. She opens the deodorant, they jokingly debate whether they like the scent.
Mauro is 27, has hazel eyes and a boyish face, but it’s one that also appears to be worn from years of drug use. He’s missing part of a front tooth. He says naloxone has saved his life a lot, starting with his very first shot of heroin on his birthday in 2011.
“I was in Bucks County at my dad and mom’s house,” he recalled.
Mauro says he’s often felt numb to it all, rotating in and out of treatment, but amid that, he’s also saved other people’s lives administering naloxone. And, he says, since that first overdose, Naloxone has brought him back over a dozen times.
“It’s above average,” he said.
Rostucher turns to him in the backseat and chimes in.
“And look at him, he’s worth it,” she tells him. “Without it, Sal wouldn’t be here. We wouldn’t have Sal, right? Sal’s moving forward, making strides.”
The last time Mauro overdosed and then received naloxone was over six months ago. Rostucher drops him off at his recovery house, where he’s now figuring out the more long term ‘what’s next’ questions, like what about a job and permanent housing.
Mauro smiles, he says Rostucher has always been a non-judgmental, trusting figure. She was the one he reached out to for help.
She drops him off at his recovery house, but not before giving him a hug.
“Call me if you need anything,” she tells him.
Rostucher started out as a volunteer, but she’s since formed her own organization, Angels in Motion. She has an army of more than 200 volunteers.
Holly Platts – who last overdosed in October, only to find Rostucher waiting for her when she left the hospital – is one of them.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.



