Light may be the key to treating diabetes with fewer needles
Listen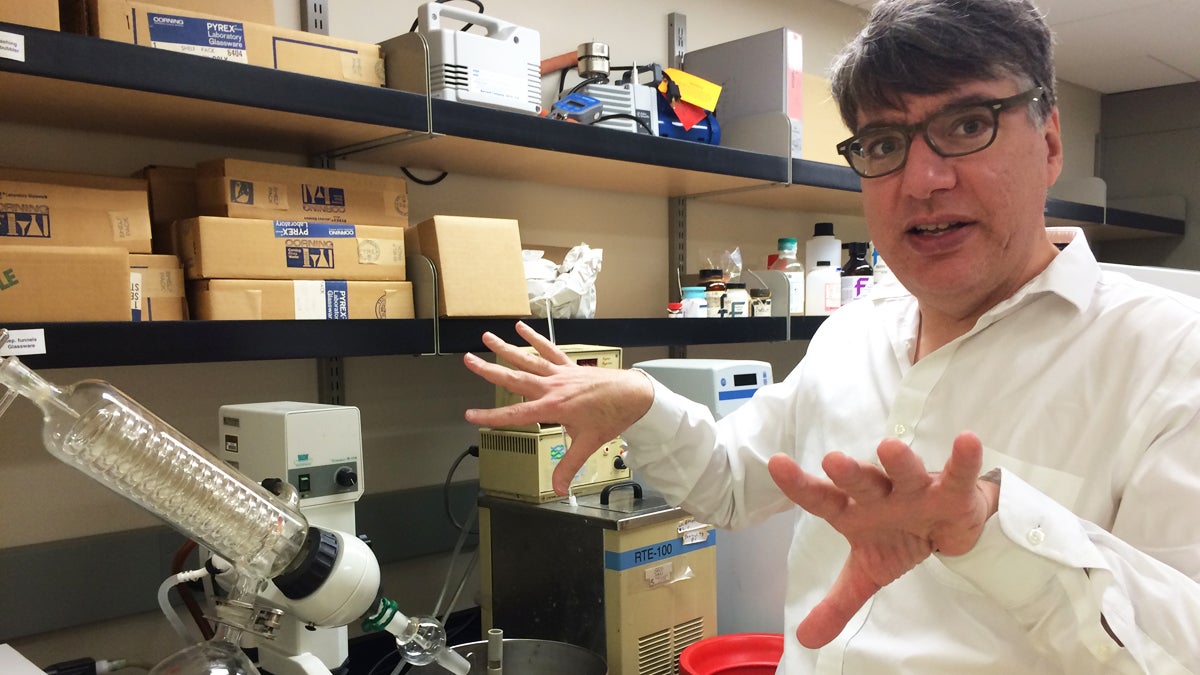
Professor Simon Friedman of the University of Missouri-Kansas City school of pharmacy is developing an alternate method of delivery insulin. (Alex Smith/for WHYY)
For diabetics with an aversion to needles, there may be light at the end of the tunnel. Literally.
On a busy league night in a Raytown, Missouri bowling alley, former auto worker Raymond Fowler keeps his game up playing alongside his wife and long-time teammates.
Fowler, who’s in his 60s, stays busy in his retirement, but it’s not all fun. A few years ago, he was diagnosed with type 2 diabetes and made a lot of changes to his diet and exercise routine, which now includes four bowling sessions per week.
His condition was severe enough that his doctor said he needed insulin shots, and that’s one change he’s had trouble with.
“The insulin—it would burn when you’d shoot yourself. It would just sting,” Fowler says. “And so after a while I went back and talked to my endocrinologist and told her, ‘I can’t keep doing this the rest of my life.'”
Insulin is a protein and can’t be taken orally in a pill because the body would try to digest it. Instead, many diabetics have to inject it with a syringe or a pen to maintain healthy blood sugar levels.
The routine can be especially complicated for type 1 diabetics, who have to test glucose levels and adjust insulin levels many times a day.
To reduce the hassle, discomfort, and pain these diabetics endure, professor Simon Friedman of the University of Missouri-Kansas City school of pharmacy is developing an alternate method of delivery insulin.
In preference to needles, his approach would pierce the skin with light, which, rather than diabetes itself, was the original inspiration for his work.
“It started with light,” he says. “We had quite a few years of developing methods to control other biological processes.”
On a recent afternoon in his lab, Friedman showed a rough prototype of an LED device that he says could be used to trigger the release of insulin. It’s a project that recently won a grant of nearly $1.5 million dollars from the National Institutes of Health.
Instead of needles, light
His idea is to create a single injection that would contain many individual insulin doses held together in a resin using “photocleavable linkers”—special molecular bonds that are especially sensitive to light.
“They’re molecules that do chemistry when you shine light on them,” Friedman says. “They’re kind of related to the molecules you might find in a recordable CD or DVD. They undergo photochemistry—chemistry bonds being made and broken using light.”
These light-sensitive bonds have been used in fields like genetics for a few years, but they’re new to pharmaceuticals.
Friedman envisions a method in which a patient would inject the insulin mixture under the skin and strap an LED light atop it. When a glucose monitor indicates insulin is needed, the light would shine through the skin and break the link between the resin and the insulin, freeing the insulin to enter the bloodstream.
Unlike injections spread out over the course of a day, this approach would adjust insulin levels constantly.”That’s the nice thing about light,” Friedman says. “You can continuously vary light. Second by second, you can adjust the intensity of light. You can change the duration of a light, and with that you can get continuously variable changes in release.”
Friedman hopes this method will cut required injections down to once every few days, once a week, or possibly every few weeks.
The goal of reducing needle injections has spawned an entire field of research within diabetes care, and the value of this work extends beyond simply making injections more comfortable.
Less needles, healthier patients
Mark Peyrot, a sociology professor at Loyola University Maryland in Baltimore who studies quality of life issues for diabetics, says that fewer painful injections can mean greater adherence to regimens and better health for patients.
That what happens when patients use insulin pens, which we were introduced as a less painful alternative to syringes about 30 years ago.
“They tend to find it more convenient, so they are more comfortable in taking their medication, which may make it somewhat more likely or easier for them to begin taking insulin or to take more shots if they have to take shots in the day,” Peyrot says.
To get patients on board with new insulin technology, however, it has to be simple and streamlined, unlike some recent delivery systems like insulin pumps and inhalable insulin, which haven’t really taken off.
“Anytime you ask a patient to change from what they’re already doing to something else, there’s barriers,” Peyrot says. “There’s just inertia there. Learning something new, learning about a new device, finding out about it – creates a barrier.”
Still a way to go
The new insulin system may be promising, but Peyrot sees a couple of wrinkles that may need working out.
The light and insulin method is meant to work hand-in-hand with a constant glucose monitoring system, and that technology isn’t quite perfected yet.
Even if it is, it would probably have to be worn, along with the light emitter itself, on the outside of the body and for some, that could be a deal breaker.
“Patients also sometimes have concerns that have more to do with cosmetics—things like being concerned what they like look like if they have a device attached to their body,” Peyrot says.
Friedman says there’s still plenty of work to be done on the technology. Early tests using animals have been encouraging, but he’ll spend the next few years refining it to find the optimal insulin mixture and light usage.
Whatever form it takes, insulin delivery without regular injections can’t come soon enough, as far as Raymond Fowler is concerned.
Exercise, diet and oral medications have allowed him to stop taking insulin, but his blood sugar is creeping up again, and he’s now facing the possibility of having to start injections all over again.
He confesses he’s been putting off some doctor’s visits.
“That’s the reason why at first I didn’t want to go to see her, because I knew she’d put me back on insulin,” Fowler says. “And I just couldn’t fool with them needles no more.”
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.



