‘Work hard and quick, but be careful’: Rushing to create a coronavirus vaccine
Despite the challenges, there are many candidates to be the vaccine that knocks out the coronavirus. But are they all equally promising?
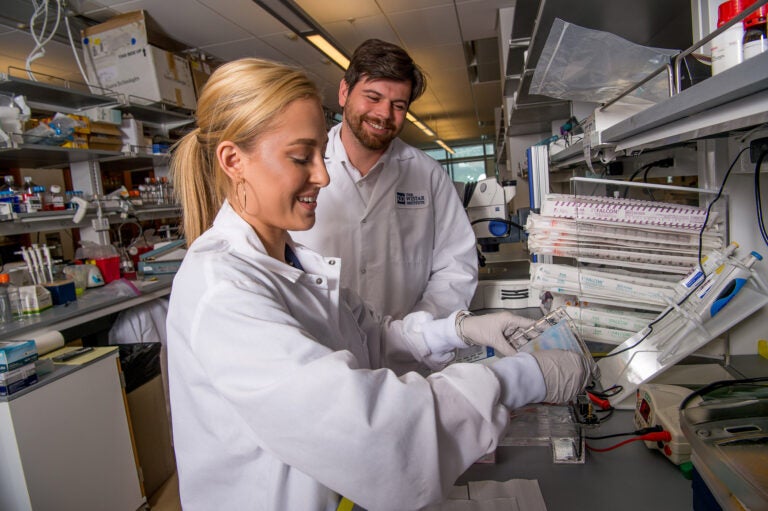
Dr. Dan Kulp, associate professor in Wistar’s Vaccine & Immunotherapy Center, works with a member of his lab. (Courtesy of The Wistar Institute)
Are you on the front lines of the coronavirus? Help us report on the pandemic.
A vaccine against the coronavirus that causes COVID-19 would be, without a doubt, one of the most highly anticipated medical discoveries of 2020.
Just what will be injected into our arms to provide immunity to the new virus officially known as SARs-CoV-2? That won’t matter to most of us, as long as it works. Getting there is the battle right now.
“So [the] perfect vaccine is single shot, needle-free, thermo stable, lifelong immunity, cheap to produce,” said Matthias Schnell, chair of microbiology and immunology at Thomas Jefferson University, whose team has been developing a COVID-19 vaccine on a rabies vaccine vector.
“Does anybody have it? I don’t think so, necessarily,” Schnell said.
Making a vaccine is hard, and lots of the possible candidates will fail during research, development, or safety testing.
A March 20 report from the World Health Organization listed two vaccines in Phase I trials, the first step in testing an experimental drug in humans, and 42 preclinical candidate vaccines. Since then, a candidate from Plymouth Meeting-based Inovio has moved into Phase I trials as well. A vaccine developed by Massachusetts-based Moderna, that was in Phase I trials as of March 20, is adding more people.
Meanwhile, CanSino Biologics, a China-based vaccine manufacturer, has advanced its vaccine into Phase II trials with people who have COVID-19. And other big companies are throwing their hats in the ring.
Researchers have had the data they needed to get started since January 11. Some worked on SARS, which is also caused by a coronavirus, and so they had some idea what they were dealing with. But the often-cited 18-month minimum time to develop a new vaccine is no joke, even when the urgency is great.
“This is a lot of doses you have to produce. So we have to work hard and quick, but be careful,” said Schnell.
Aside from the logistics of making enough doses of a vaccine for every American, there are the very real science issues. A vaccine needs to create strong immunity that helps your body recognize and fight off the virus. But before it becomes available to all of us it also needs to be safe and successfully pass through the three-phase trial system that ensures that it has been tested and proven to work.
A crash course in immunology
Even though all working vaccines give you some sort of immunity, all vaccines aren’t equally good at provoking it.
“Some vaccines cause weak immune responses and they require multiple doses, and other vaccines really don’t elicit a sufficient response at all.” said Daniel Kulp, a professor at Philadelphia’s Wistar Institute. He works with nanoparticles, which he thinks could lead to better vaccines — “we use these nanoparticles to drive stronger immunity.”
“Nanoparticles are usually virus-size molecules that can be used to display multiple copies of your vaccine on the surface,” Kulp said.
The human body has immune cells that recognize intruders. In the case of a new intruder, the immune cells take a biological fingerprint called an antibody. These antibodies help your body keep track of any viruses it’s been exposed to.
When you get a vaccine, you’re priming your immune system. Imagine a police department getting hold of only the hand of an intruder. The hand gives the police fingerprints so they can identify the intruder, but the hand itself isn’t dangerous. That’s why most vaccines only use a tiny part of the virus, called the antigen (the metaphorical severed hand) to generate that fingerprint.
If you actually get the virus with no vaccine and get better, it’s as if you’ve been exposed to the whole intruder, and you’ve generated fingerprints (antibodies) the same way. Once you have these antibodies, you hold on to them, at least for a while, and they protect you.
There isn’t a nanoparticle vaccine for COVID-19 yet. Kulp has been collaborating with the Weiner lab also at the Wistar Institute. The Wistar is an independent nonprofit research organization that has been involved in several vaccines. The Weiner lab contributed intellectually to the Inovio vaccine currently in Phase I trials. Phase I trials are often with a small group of young, healthy people. If it passes, the next step will be a bigger, more representative group.
The Inovio vaccine is a DNA vaccine. If you thought nanoparticles sounded like science fiction, buckle up your warp drive.
Vaccines like this safely put a little strip of DNA called a plasmid into some of your cells. This plasmid is like a recipe: Your cells read out the DNA and follow the recipe to make a protein, in this case, the antigen — the severed hand in the nanoparticle example. In a way, a DNA vaccine is the ultimate DIY.
Wistar’s Weiner lab uses the spike protein, the same protein SARs-CoV-2 uses to sneak inside your cells.
“So when we deliver this DNA plasmid into animals or people, all you see is just the spike protein, and your body develops an immune response against just that one target,” said Ami Patel, a research assistant professor at the Weiner lab.
What does this mean for you, the potential consumer? If the DNA vaccine makes it the whole way through development, what’s known as going from bench to bedside, it would be the first DNA vaccine widely available. Apart from a special needle, engineered by Inovio, getting a DNA vaccine would be exactly like getting any other vaccine.
“I think right now everybody’s just focused on making sure that all of the vaccines that we’re collectively generating are safe. I think that’s the main focus.” said Patel. “Once we get past that focus, then it’s really how to expedite this to the general population.”
Logistics are a huge part of a successful vaccine, which gives the DNA vaccine a bit of an edge.
“Plasma DNA is very quick to produce, and in terms of stability, it’s quite stable,” said Patel. The plasmid is stable for several years in a refrigerator and a year at room temperature.
That’s not the case with all vaccines. During the West African Ebola epidemic, even though there was a vaccine, it needed to be kept in cold storage, at -80 degrees Celsius to work, Patel said. For reference, your freezer is a warm -20 degrees Celsius.
Non-vaccine possibilities
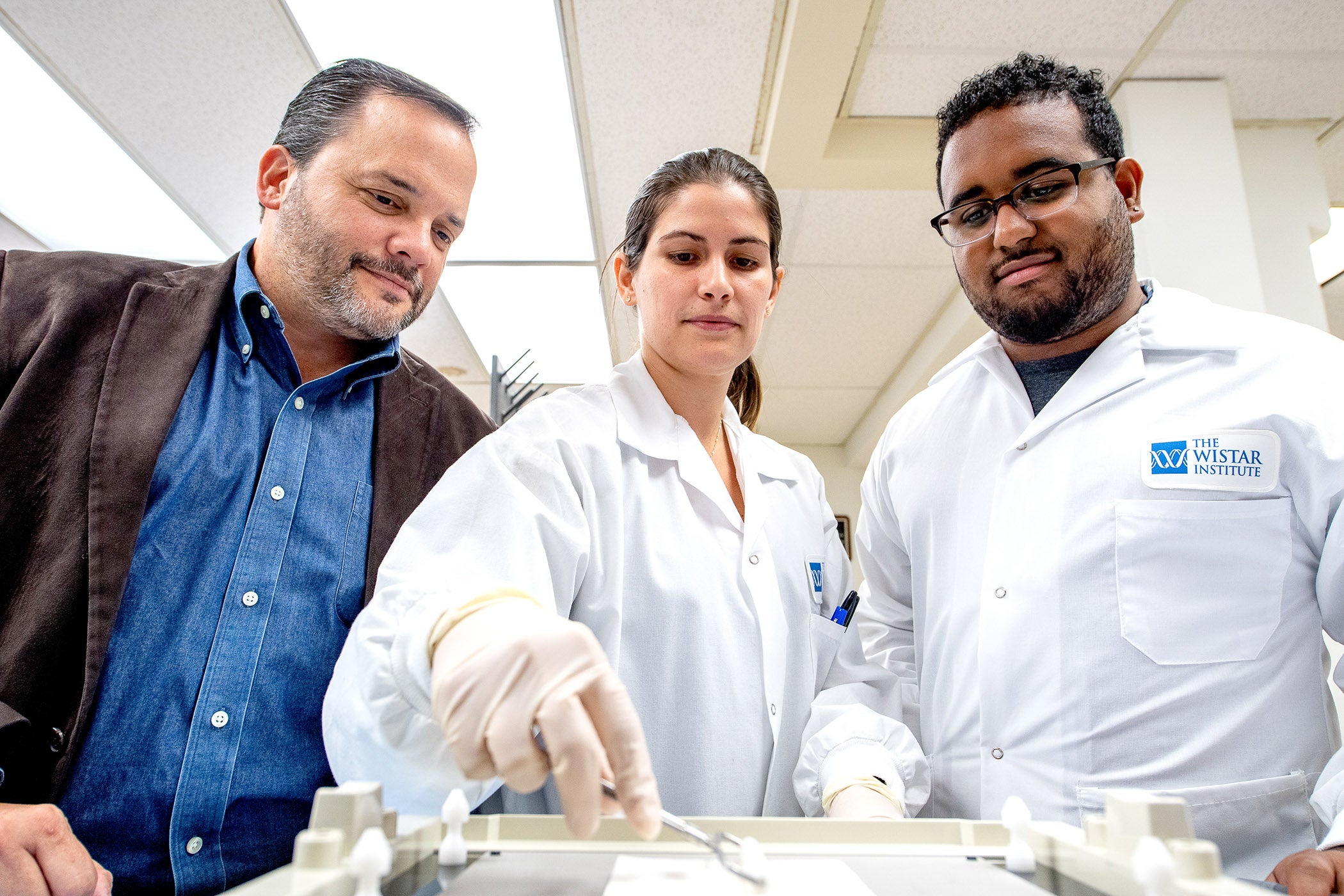
A vaccine isn’t the only potential solution, as scientists such as Luis Montaner and Joseph Salvino pivot their research.
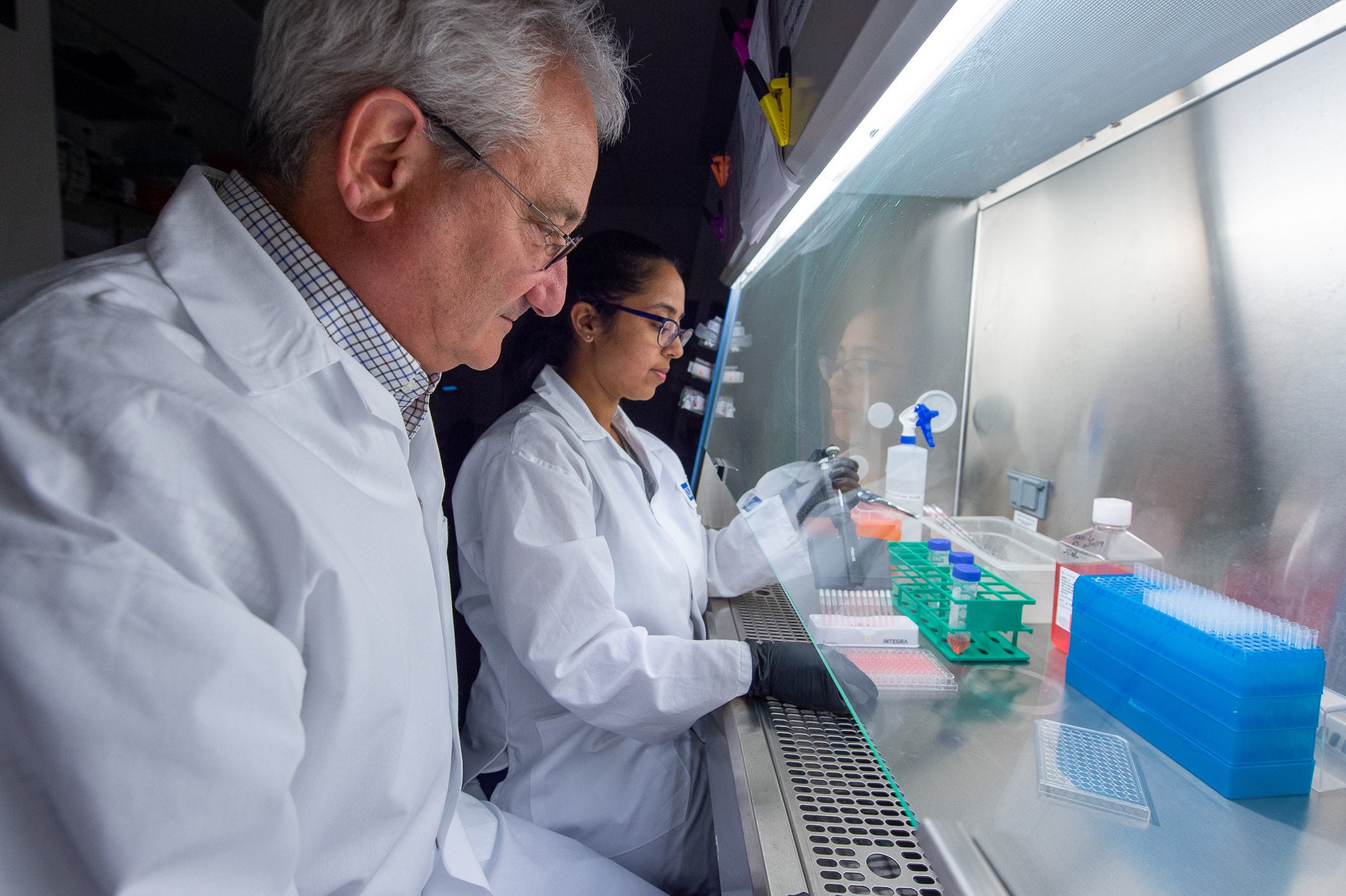
Salvino is scientific director of the Molecular Screening & Protein Expression Facility at Wistar. Montaner is the director of the HIV-1 Immunopathogenesis Laboratory and leader of the HIV Research Program in Wistar’s Vaccine & Immunotherapy Center. Before COVID-19, they studied small molecules that would help treat chronic immune activation coming from something called interferon. “So we set up almost three years’ worth of infrastructure to try to identify, and we have identified, molecules that can … block the interferon response,” said Montaner.
In the case of COVID-19, however, that interferon response is a good thing. So they turned their research on its head. From their initial search for molecules, Salvino and Montaner had some that they discarded, because instead of suppressing the interferons, they activated them. Those are the molecules they are now turning into therapeutics for COVID-19, and other viral infections.
This attitude, a willingness to drop what you were working on and switch to COVID-19, is not uncommon — “because everyone’s trying to move very fast and try to help, everyone’s just trying to pitch in to do what they can, and it’s great.” said Kulp.
Some of the vaccines that are in development are DNA and RNA vaccines, which will be new technology for everyone. Many are recombinant vaccines, which will use a bit of SARS-CoV-2 protein to provide the same chance to develop immunity with no risk of infection because it isn’t the whole virus.
“There’s not a single silver bullet, a way of making a vaccine right now. So everyone has smart ways of doing it, and everyone should be trying, in my opinion, everyone should be trying those to get us to a place where we have a vaccine and therapies as fast as we can.” said Kulp.
But the type of vaccine won’t be as important as the fact that we have one. Although people can respond differently to the same vaccine, testing that is what clinical trials are for. If ultimately there are multiple vaccines, those will be conversations to have with your doctor.
Can you, as a non-scientist, do anything to help?
Yes, according to Kulp: There’s a game called Foldit that lets non-researchers help solve protein-folding problems.
Proteins are made of lots of little building blocks, and kind of like starting with a box of hundreds of Lego pieces, there are tons of possible structures. Foldit lets you try to predict the best possible structure, something that, according to Foldit’s website, will save time and money.
So it’s a chance to do your part, even if you’re not in drug R&D, or working an essential job or delivering supplies. Maybe you’re sitting at home, social distancing. Since you’re already there, maybe doing a little gaming, you could give it a shot.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.



![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)



