The vaccines work against severe disease. Here’s why boosters are still a good idea
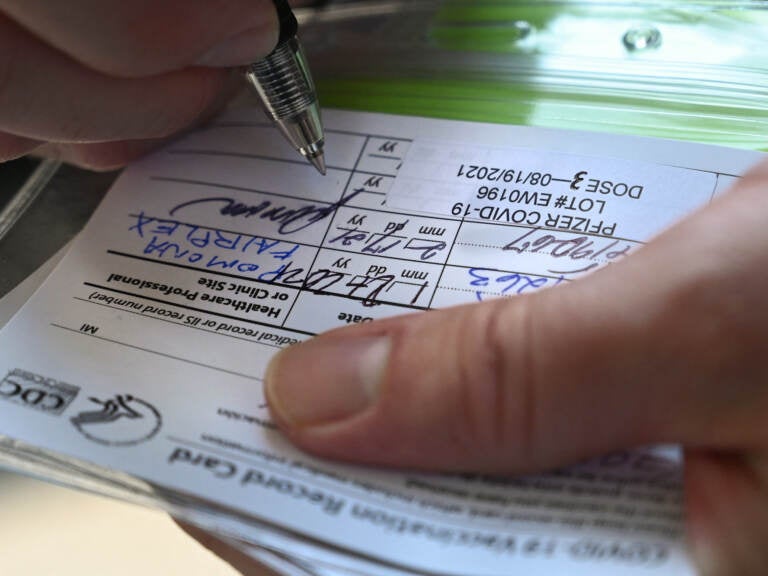
Health authorities have been urging Americans to get a booster shot six months after their second dose of the vaccine, especially now that the omicron variant is dominant in the U.S. (Robyn Beck/AFP via Getty Images)
Several nights ago, my husband, who was traveling, texted me these questions:
Does my vaccine not work anymore?
Should I get a booster even though it’s been only four months since my second shot?
“Excellent questions,” I thought as I read his texts. One thing is crystal clear about the highly-mutated variant: It has a huge ability to bypass immune protection and cause breakthrough infections.
Here’s what you need to know about how well the vaccines are working in the face of the omicron variant, and the best timing for getting your booster shot.
1. Does my COVID vaccine not work anymore?
Yes and no.
Two shots of a vaccine – whether it’s Pfizer, Moderna – do still offer protection against severe disease, researchers in South Africa have found. In a study with about 78,000 omicron cases, getting two shots of Pfizer cut a person’s risk of hospitalization by about 70% across all age groups. That’s compared with a 90% reduction of risk with delta, but it does indicate that the vaccines are still working really well to keep people out of the hospital. The effectiveness against omicron seems to hold up in older people as well, although it declines a bit, to about 60%.
But when it comes to stopping an infection, two shots isn’t enough, the researchers found. The vaccine’s effectiveness against an infection with omicron was only about 30%, which means breakthrough infections will be extremely common with this new variant.
2. How much does the booster help?
Probably a lot – against infection.
The problem with only two shots of the vaccine is that most of the antibodies your body generates don’t have the potency to neutralize omicron when it first attacks your upper respiratory tract. That means you could easily get a breakthrough infection. (The good news is that for most people, the immune system does kick in to fight off severe disease, once memory cells activate.)
Laboratory studies have shown that antibodies, after only two shots, are 40 to 50 times less potent against omicron than against previous variants.
“We found that only 32% of people who received Moderna, even if it was recently, had detectable neutralization ability against omicron,” says immunologist Wilfredo Garcia Beltran, who’s a fellow at the Ragon Institute of Massachusetts General Hospital.
But after the booster shot, that percentage goes up dramatically, he says: “If you boost everyone, the numbers look amazing.”
After the booster shot, the amount of neutralization potency against omicron rose up to a level close to what Garcia Beltran observed against the delta variant. “I think this finding is suggestive that we’re inducing really good neutralization against omicron with a booster,” he says.
And those laboratory findings fit with what health officials have observed in the U.K.: “Moderate to high vaccine effectiveness of 70 to 75% is seen in the early period after a booster dose,” the U.K. Health Security Agency reported two weeks ago.
Altogether, these studies show that a third dose gives you the best chance of preventing an omicron infection this winter. For some young and healthy people, catching a mild case of omicron might not be that big of a burden, but a booster still reduces your risk of spreading it to older loved ones or other vulnerable people.
“We definitely need to give this to everyone if we want to prevent omicron from spreading like wildfire – or at least, curtail its spread,” Garcia Beltran adds.

3. I got my primary dose four months ago and was told to wait until six months. Do I have to wait, or can I get a booster now?
Officially, adults are eligible for a booster two months after the J&J vaccine and six months after Pfizer or Moderna. Right now, that’s still the official recommendation.
However, because two shots provides such little protection against an infection with omicron, doctors and scientists are shifting their recommendation a bit about the timing of the booster after the mRNA vaccines.
“In the setting of a new variant – and wanting a higher degree of protection for the holidays, then I do think that clinical judgment could involve boosting a bit earlier,” says Dr. Daniel Barouch, who runs the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center in Boston.
The original six month recommendation is based on “the ideal spacing between three-dose vaccine regimens,” Dr. Monica Gandhi, who’s an infectious disease specialist at the University of California, San Francisco, in an email to NPR. “Zero, one and six months is what we use for so many three-dose vaccines.”
But with omicron about to surge, she says, getting a boost in antibodies earlier might be worth it.
“There is probably no harm in speeding up to boost antibodies,” she writes, just as long as you wait at least three months from the second shot.
This is especially true for people who are at high risk for severe disease or live with someone who is.
In fact, Germany’s vaccine authority recently recommended that Germans get their boosters after three months, in light of omicron.
But Barouch cautions against speeding up the booster too much.
“I wouldn’t boost too much earlier,” he says. “For example, I wouldn’t boost a month or two after the initial vaccine or vaccines. But if somebody is in the second half of the six month timeframe, and if they really feel like they would benefit from a higher level of protection, then I don’t see a downside in getting boosted a bit earlier.”
4. How does a booster work to improve protection against a new variant like omicron? And why do we have to wait several months to get one?
Improved immunity is not just about having more antibodies; it’s also about having the kind of antibodies that can actually take down omicron. For your body to generate those specific antibodies, it takes time – we’re talking at least three months after the first two shots.
You see, right after your first two shots of the vaccine, your immune system rushes and makes a burst of antibodies. But these antibodies aren’t so great. They especially aren’t good at fighting off new coronavirus variants, says immunologist Ali Ellebedy at the Washington University School of Medicine. “That initial group isn’t very well trained.”
The level of these antibodies starts to go down after about a month, and then your body gets to work to “train” these antibodies, Ellebedy says. Special immune cells, called B cells, go into your lymph nodes and start to improve the potency of the antibodies. Eventually, over time, through a process called B cell maturation, these B cells develop new antibodies that not only can recognize and neutralize the original variant of virus (which it saw in the vaccine) but also future variants, such as omicron.
“To protect you from future exposures, you want to have the best, well-equipped ‘soldiers,’ and the way our immune system does this is through this process of refinement in our lymph nodes,” Ellebedy says.
“This process takes time. It can take months.”
But if you get a booster before this process is finished, the shot will essentially amplify the “untrained” antibodies.
So if you wait at least three months, the third dose of the vaccine will amplify the “well-trained” antibodies, which are potent against not just omicron, but also possibly the next variant after that.
“There are studies that do show that the longer the period between vaccinations, the more robust the response to second immunization and that makes sense immunologically,” Ellebedy writes in an email to NPR.
“However, that does not mean that an earlier immunization will not be beneficial or harmful in any way. Actually, in the middle of a pandemic one can argue that a three-month or four-month booster makes more sense,” she adds. “Getting that before being exposed to the real virus is always a plus.”

5. How fast will the booster work?
The boosters work a bit faster than the original course of the vaccine, because your body isn’t starting from scratch, says Dr. Simone Wildes, who’s an infectious disease doctor at South Shore Health in Massachusetts.
“You already have some antibodies,” she says. “So I would anticipate that within a week or so after the booster, you’re going to have pretty significant levels of antibodies, but you’re not going to get to the maximum levels until the 14-day mark.”
So if you go get vaccinated today, you will have some antibody protection by New Years.
6. How long will the protection from the booster last?
Nobody knows how long protection from infection will last. One preliminary study suggests it will start to wane about three months after the booster shot, as has been the case with the delta variant.
There’s no information about how long protection against severe disease will last after a booster, but given the durability observed with only two shots, it’s likely to be quite durable – much more than protection against infection.
9(MDAzMzI1ODY3MDEyMzkzOTE3NjIxNDg3MQ001))



![CoronavirusPandemic_1024x512[1]](https://whyy.org/wp-content/uploads/2020/03/CoronavirusPandemic_1024x5121-300x150.jpg)

